filmov
tv
How Medical billing works

Показать описание
Medical billing is the process of submitting and following up on claims with health insurance companies in order to receive payment for healthcare services provided to patients. Revenue Cycle Management (RCM) refers to the entire process of managing a healthcare provider's revenue cycle, from the moment a patient makes an appointment to the time the provider receives payment for services rendered.
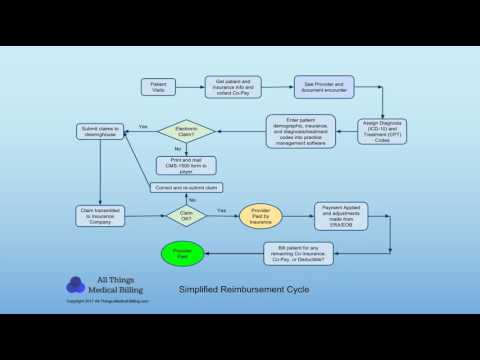
The medical billing RCM cycle involves a series of steps that healthcare providers must follow in order to get paid for their services. The following are the steps involved in the medical billing RCM cycle:
Patient Registration: The first step in the medical billing RCM cycle is patient registration. This involves collecting the patient's personal and insurance information, which will be used to bill the insurance company for the services provided.
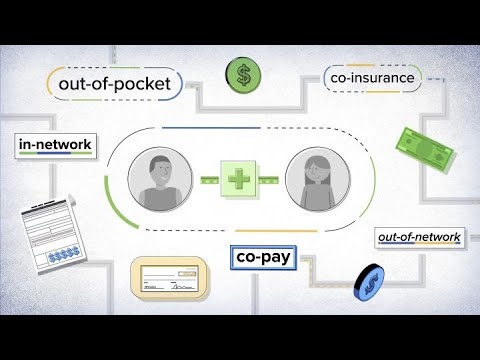
Eligibility Verification: Before providing services, the healthcare provider must verify the patient's insurance coverage and benefits. This step is important because it helps to avoid claim denials or delays in payment.
Charge Capture: Once the patient receives medical services, the provider must document the services provided and the associated charges. This information is then used to create a claim to submit to the insurance company.
Claim Submission: After the charge capture process is complete, the provider must submit a claim to the insurance company. This can be done electronically or through paper submission, depending on the insurance company's requirements.
Claim Adjudication: After the claim is submitted, the insurance company reviews the claim and determines whether it will be paid or denied. If the claim is denied, the healthcare provider must identify the reason for denial and resubmit the claim.
Payment Posting: Once the claim has been accepted and paid by the insurance company, the payment is posted to the patient's account in the provider's billing system.
Denial Management: If a claim is denied, the healthcare provider must identify the reason for denial and work to correct the issue. This may involve appealing the claim or working with the insurance company to resolve the issue.
Patient Collections: If the patient is responsible for paying a portion of the bill, the healthcare provider must collect payment from the patient. This can be done through various methods, such as sending a bill in the mail, collecting payment at the time of service, or setting up a payment plan.
Overall, the medical billing RCM cycle is a complex process that requires a great deal of attention to detail and expertise. By following these steps, healthcare providers can ensure that they are paid for the services they provide and that patients are billed accurately and efficiently.
The medical billing RCM cycle involves a series of steps that healthcare providers must follow in order to get paid for their services. The following are the steps involved in the medical billing RCM cycle:
Patient Registration: The first step in the medical billing RCM cycle is patient registration. This involves collecting the patient's personal and insurance information, which will be used to bill the insurance company for the services provided.
Eligibility Verification: Before providing services, the healthcare provider must verify the patient's insurance coverage and benefits. This step is important because it helps to avoid claim denials or delays in payment.
Charge Capture: Once the patient receives medical services, the provider must document the services provided and the associated charges. This information is then used to create a claim to submit to the insurance company.
Claim Submission: After the charge capture process is complete, the provider must submit a claim to the insurance company. This can be done electronically or through paper submission, depending on the insurance company's requirements.
Claim Adjudication: After the claim is submitted, the insurance company reviews the claim and determines whether it will be paid or denied. If the claim is denied, the healthcare provider must identify the reason for denial and resubmit the claim.
Payment Posting: Once the claim has been accepted and paid by the insurance company, the payment is posted to the patient's account in the provider's billing system.
Denial Management: If a claim is denied, the healthcare provider must identify the reason for denial and work to correct the issue. This may involve appealing the claim or working with the insurance company to resolve the issue.
Patient Collections: If the patient is responsible for paying a portion of the bill, the healthcare provider must collect payment from the patient. This can be done through various methods, such as sending a bill in the mail, collecting payment at the time of service, or setting up a payment plan.
Overall, the medical billing RCM cycle is a complex process that requires a great deal of attention to detail and expertise. By following these steps, healthcare providers can ensure that they are paid for the services they provide and that patients are billed accurately and efficiently.
Комментарии
 0:14:03
0:14:03
 0:05:53
0:05:53
 0:04:29
0:04:29
 0:03:43
0:03:43
 0:07:28
0:07:28
 0:03:59
0:03:59
 0:03:12
0:03:12
 0:02:33
0:02:33
 2:11:35
2:11:35
 0:14:07
0:14:07
 0:44:12
0:44:12
 0:00:06
0:00:06
 0:00:52
0:00:52
 0:01:27
0:01:27
 0:10:29
0:10:29
 0:07:57
0:07:57
 0:00:37
0:00:37
 0:16:22
0:16:22
 0:05:34
0:05:34
 0:04:20
0:04:20
 0:04:57
0:04:57
 0:00:56
0:00:56
 0:05:35
0:05:35
 0:00:57
0:00:57