filmov
tv
Cervical Spine Trauma - Everything You Need To Know - Dr. Nabil Ebraheim
Показать описание
Dr. Ebraheim’s educational animated illustrates spine concepts associated the cervical spine - trauma.
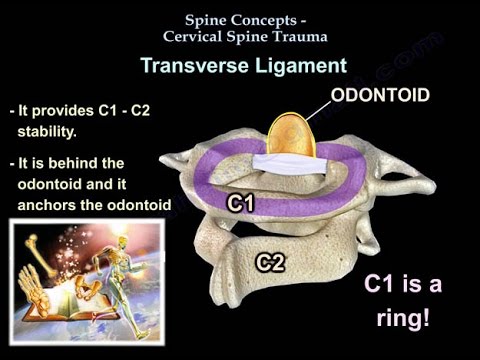
Transverse ligament:
- It provides the C1-C2 stability
- It is behind the odontoid and it anchors the odontoid to the ring of C1 so it prevents an abnormal movement between C1 and C2.
- A.D.I. in adults is 3.5 mm.
- Of the transverse ligament is injured, C1 and C2 will be free to move & there will be an increase in the A.D.I.
- Isolated traumatic injury to the transverse ligament is probably rare.
- Jefferson fracture
Three types:
- Type II: fracture at the base of the odontoid process, most common, troublesome fracture.
- Nonunion rate is 20-80% due to interruption of the blood supply.
- High nonunion rate in:
- More than 5 mm of displacement.
- Patients older than 50 years of age.
- Other risk factors:
- Delay in treatment
- Posterior displacement of the fracture
- Diabetes
- Do not use halo in early patients, risk of death from pneumonia
- Treatment of young patients:
• Halo: halo traction may be needed initially to reduce fracture, halo for up to 3 months, 30% non-union rate in halo.
• When do you do surgery? Displaced fracture in older patients, risk factors for no-union.
• Odontoid screw is preferred in the young patient.
• Need to preserve C1-C2 motion.
• Do not do fusion in young patients.
• Can use C1- C2 fusion in older patients.
• For older patients:
- Orthosis or Fusion of C1- C2 if there is an indication for surgery and if there is a clearance for surgery.
Type III:
- Fracture through the body of C2.
- Treatment:
• Cervical orthosis
• Halo: if displaced
• Hangman’s fracture is a bilateral fracture of the pars interarticularis
• The spinal canal is wider and there will be a low risk for spinal cord injury.
Levine and Edwards classification:
- Type I: stable fracture with less than 3 mm displacement, no angulation, treatment: cervical orthosis.
- Type II: most common type, significant translation and some angulation, unstable fracture, treatment: cervical traction and extension to improve the displacement, immobilization in halo vest for about 3 months.
- Type IIa: severe angulation and slight translation seen in flexion distraction injuries with tearing of the posterior longitudinal ligament, the fracture is unstable, treatment: do not use traction when there is severe angulation of the fracture.
- Type III: surgical type, C2-C3 facet dislocation, rare fracture of the pedicles in addition to the anterior facet dislocation, it has some neurological deficit association, treatment: surgery for reduction of the facet dislocation and stabilization of the injury, open reduction and posterior spine fusion.
• Facet dislocations: the association of disk herniation and facet involvement is very high, so watch out for a herniated disc in addition to the bony injury.
- Unilateral facet dislocation will usually have less than 50% translation on x-ray and it may affect a nerve root.
- Bilateral facet dislocation will have more than 50% translation and probably a spinal cord injury.
- Treatment: immediate closed reduction, get an MRI, then do surgery, if the patient has a change in mental status, then get the MRI first, and immediately followed by open reduction and surgical fixation.
- When do you go anteriorly?
- Go anteriorly if there is a disc herniation, incidence is about 10%-30% in cervical facet dislocation.
- If you try to do reduction, the disc fragment may stay in the canal causing spinal cord injury.
- When do you do posterior?
- If reduction of the dislocation failed and there was no disc herniation.
- When do you combined anterior and posterior procedures?
- Need to go anteriorly to remove the disc
- Need to go posteriorly because the dislocation cannot be reduced by a closed method or by an open anterior technique.
• Important points:
1- Get the MRI before surgery: make sure there is not a disc herniation.
2- Ligament injuries do not heal: will need fusion surgery.
3- Know the arrangement of the facets: superior and inferior facets in normal, subluxed, and dislocated positions.
Know the “naked facet” or the “empty facet”.
Train yourself to know this, especially for exam questions.
Naked Facet.
Cervical Spine MRI
Facet Fracture
Ligamentous Injury OF THE Cervical Spine
Burst Fracture of Lower Cervical Spine
Tear Drop Fracture
Follow me on twitter:
Donate to the University of Toledo Foundation Department of Orthopaedic Surgery Endowed Chair Fund:
Transverse ligament:
- It provides the C1-C2 stability
- It is behind the odontoid and it anchors the odontoid to the ring of C1 so it prevents an abnormal movement between C1 and C2.
- A.D.I. in adults is 3.5 mm.
- Of the transverse ligament is injured, C1 and C2 will be free to move & there will be an increase in the A.D.I.
- Isolated traumatic injury to the transverse ligament is probably rare.
- Jefferson fracture
Three types:
- Type II: fracture at the base of the odontoid process, most common, troublesome fracture.
- Nonunion rate is 20-80% due to interruption of the blood supply.
- High nonunion rate in:
- More than 5 mm of displacement.
- Patients older than 50 years of age.
- Other risk factors:
- Delay in treatment
- Posterior displacement of the fracture
- Diabetes
- Do not use halo in early patients, risk of death from pneumonia
- Treatment of young patients:
• Halo: halo traction may be needed initially to reduce fracture, halo for up to 3 months, 30% non-union rate in halo.
• When do you do surgery? Displaced fracture in older patients, risk factors for no-union.
• Odontoid screw is preferred in the young patient.
• Need to preserve C1-C2 motion.
• Do not do fusion in young patients.
• Can use C1- C2 fusion in older patients.
• For older patients:
- Orthosis or Fusion of C1- C2 if there is an indication for surgery and if there is a clearance for surgery.
Type III:
- Fracture through the body of C2.
- Treatment:
• Cervical orthosis
• Halo: if displaced
• Hangman’s fracture is a bilateral fracture of the pars interarticularis
• The spinal canal is wider and there will be a low risk for spinal cord injury.
Levine and Edwards classification:
- Type I: stable fracture with less than 3 mm displacement, no angulation, treatment: cervical orthosis.
- Type II: most common type, significant translation and some angulation, unstable fracture, treatment: cervical traction and extension to improve the displacement, immobilization in halo vest for about 3 months.
- Type IIa: severe angulation and slight translation seen in flexion distraction injuries with tearing of the posterior longitudinal ligament, the fracture is unstable, treatment: do not use traction when there is severe angulation of the fracture.
- Type III: surgical type, C2-C3 facet dislocation, rare fracture of the pedicles in addition to the anterior facet dislocation, it has some neurological deficit association, treatment: surgery for reduction of the facet dislocation and stabilization of the injury, open reduction and posterior spine fusion.
• Facet dislocations: the association of disk herniation and facet involvement is very high, so watch out for a herniated disc in addition to the bony injury.
- Unilateral facet dislocation will usually have less than 50% translation on x-ray and it may affect a nerve root.
- Bilateral facet dislocation will have more than 50% translation and probably a spinal cord injury.
- Treatment: immediate closed reduction, get an MRI, then do surgery, if the patient has a change in mental status, then get the MRI first, and immediately followed by open reduction and surgical fixation.
- When do you go anteriorly?
- Go anteriorly if there is a disc herniation, incidence is about 10%-30% in cervical facet dislocation.
- If you try to do reduction, the disc fragment may stay in the canal causing spinal cord injury.
- When do you do posterior?
- If reduction of the dislocation failed and there was no disc herniation.
- When do you combined anterior and posterior procedures?
- Need to go anteriorly to remove the disc
- Need to go posteriorly because the dislocation cannot be reduced by a closed method or by an open anterior technique.
• Important points:
1- Get the MRI before surgery: make sure there is not a disc herniation.
2- Ligament injuries do not heal: will need fusion surgery.
3- Know the arrangement of the facets: superior and inferior facets in normal, subluxed, and dislocated positions.
Know the “naked facet” or the “empty facet”.
Train yourself to know this, especially for exam questions.
Naked Facet.
Cervical Spine MRI
Facet Fracture
Ligamentous Injury OF THE Cervical Spine
Burst Fracture of Lower Cervical Spine
Tear Drop Fracture
Follow me on twitter:
Donate to the University of Toledo Foundation Department of Orthopaedic Surgery Endowed Chair Fund:
Комментарии
 0:16:37
0:16:37
 0:09:58
0:09:58
 0:03:19
0:03:19
 0:03:36
0:03:36
 0:05:57
0:05:57
 1:04:38
1:04:38
 0:02:58
0:02:58
 0:10:23
0:10:23
 0:09:20
0:09:20
 0:05:13
0:05:13
 0:01:40
0:01:40
 0:04:34
0:04:34
 0:25:31
0:25:31
 0:01:54
0:01:54
 0:35:48
0:35:48
 0:05:46
0:05:46
 0:01:51
0:01:51
 0:28:59
0:28:59
 0:02:46
0:02:46
 0:01:35
0:01:35
 0:04:50
0:04:50
 0:30:20
0:30:20
 0:25:22
0:25:22