filmov
tv
Multiple sclerosis – white spots and red flags - part 1 - Making a diagnosis

Показать описание
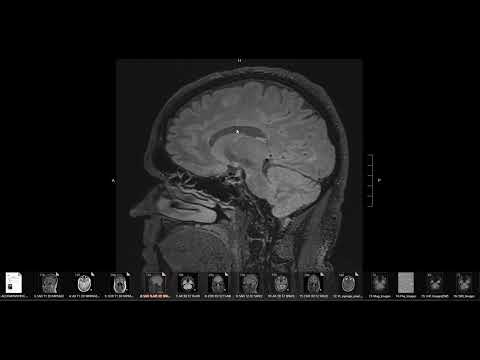
Demyelinating disease is a common situation we encounter in neuroradiology, and properly diagnosing and tracking it using MRI is a key skill for neuroradiologists. Today, Dr. Michael Hoch gives the first part of a two part lecture on how to approach white matter abnormalities in the brain and use them towards making a diagnosis of multiple sclerosis.
Multiple sclerosis is a clinical diagnosis that depends on several possible presenting signs (such as depression, fatigue, vertigo, numbness or other neurological symptoms, bladder dysfunction, visual changes, or other phenomena including L'Hermitte's sign or Uhthoff's phenomenon) and other clinical sign (including tremor, decreased perception, hyperreflexia, and ataxia).
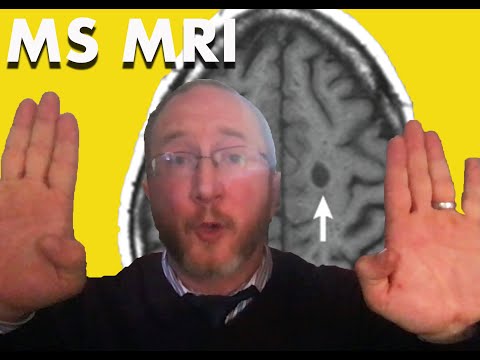
The imaging diagnosis of multiple sclerosis is based on the McDonald criteria, most recently revised in 2017. This requires dissemination in space, dissemination in time, and lack of an alternate explanation. You should evaluate different spaces for white matter abnormality, including the cortex, juxtacortical, subcortical and deep white matter, corpus callosum, and deep white matter, periventricular white matter.
The locations of the lesions can provide a clue as to whether white matter lesions are more likely to be caused by demyelinating disease or other nonspecific insults, such as chronic microvascular ischemia. For instance, central lesions in the pons or lesions in the deep white matter are more nonspecific, while cortical/juxtacortical, periventricular, and anterior temporal lesions are more specific for multiple sclerosis.
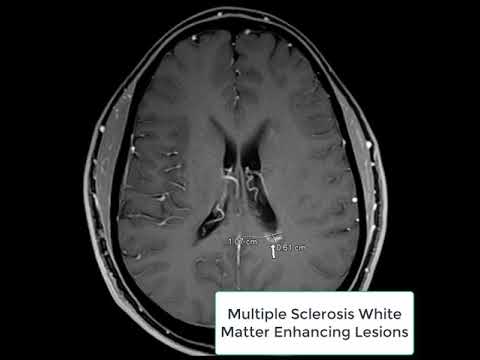
The enhancement pattern is also a clue to whether a lesion might be demyelinating. Demyelinating lesions typically have an incomplete rim of enhancement, where the post-contrast enhancement has a broken circle type of appearance. Leptomeningeal enhancement can often be seen in patients with MS, although it is an alarm bell if patients don't have a known diagnosis, as it can represent other diseases such as leptomeningeal carcinomatosis.
Key take home points of this lecture include:
Multiple sclerosis is a clinical diagnosis, not an MRI diagnosis
White spot lesion location matters
Juxtacortical lesions must touch the cortex
Aggressively window the spine to look for cord lesions
Leptomeningeal enhancement is possible in multiple sclerosis
If you haven't already, please check out part 2, in which Dr. Hoch discusses potential mimics and pitfalls when assessing for demyelinating disease.
The level of this lecture is appropriate for radiology residents, radiology fellows, and trainees in other specialties who have an interest in imaging or treating patients with potential demyelinating diseases.
Multiple sclerosis is a clinical diagnosis that depends on several possible presenting signs (such as depression, fatigue, vertigo, numbness or other neurological symptoms, bladder dysfunction, visual changes, or other phenomena including L'Hermitte's sign or Uhthoff's phenomenon) and other clinical sign (including tremor, decreased perception, hyperreflexia, and ataxia).
The imaging diagnosis of multiple sclerosis is based on the McDonald criteria, most recently revised in 2017. This requires dissemination in space, dissemination in time, and lack of an alternate explanation. You should evaluate different spaces for white matter abnormality, including the cortex, juxtacortical, subcortical and deep white matter, corpus callosum, and deep white matter, periventricular white matter.
The locations of the lesions can provide a clue as to whether white matter lesions are more likely to be caused by demyelinating disease or other nonspecific insults, such as chronic microvascular ischemia. For instance, central lesions in the pons or lesions in the deep white matter are more nonspecific, while cortical/juxtacortical, periventricular, and anterior temporal lesions are more specific for multiple sclerosis.
The enhancement pattern is also a clue to whether a lesion might be demyelinating. Demyelinating lesions typically have an incomplete rim of enhancement, where the post-contrast enhancement has a broken circle type of appearance. Leptomeningeal enhancement can often be seen in patients with MS, although it is an alarm bell if patients don't have a known diagnosis, as it can represent other diseases such as leptomeningeal carcinomatosis.
Key take home points of this lecture include:
Multiple sclerosis is a clinical diagnosis, not an MRI diagnosis
White spot lesion location matters
Juxtacortical lesions must touch the cortex
Aggressively window the spine to look for cord lesions
Leptomeningeal enhancement is possible in multiple sclerosis
If you haven't already, please check out part 2, in which Dr. Hoch discusses potential mimics and pitfalls when assessing for demyelinating disease.
The level of this lecture is appropriate for radiology residents, radiology fellows, and trainees in other specialties who have an interest in imaging or treating patients with potential demyelinating diseases.
Комментарии
 0:11:35
0:11:35
 0:17:35
0:17:35
 0:18:17
0:18:17
 0:01:23
0:01:23
 0:00:57
0:00:57
 0:11:32
0:11:32
 0:09:19
0:09:19
 0:10:22
0:10:22
 0:17:12
0:17:12
 0:01:20
0:01:20
 0:05:57
0:05:57
 0:03:15
0:03:15
 0:00:40
0:00:40
 0:58:43
0:58:43
 0:06:05
0:06:05
 0:05:41
0:05:41
 0:07:38
0:07:38
 0:26:29
0:26:29
 0:01:16
0:01:16
 0:05:45
0:05:45
 0:06:40
0:06:40
 0:04:27
0:04:27
 0:03:57
0:03:57
 0:55:20
0:55:20