filmov
tv
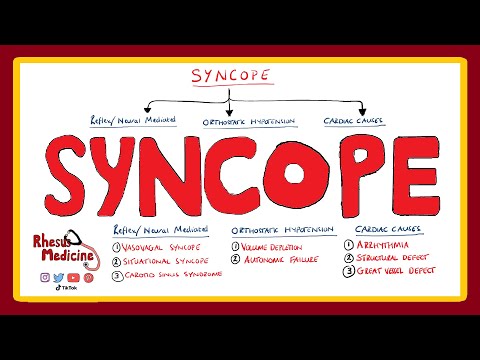
syncope - Fainting Symptoms, Causes and management

Показать описание
Syncope is transient, short-term, self-limited loss of consciousness due to acute impairment of cerebral blood flow. decrease in blood flow to the brain, typically from low blood pressure.
Characteristics of syncope.
The onset of syncope is rapid, duration is brief and recovery is spontaneous and full.
Syncope is also known as fainting or passing out.
Sometimes some prodromal symptoms occur before loss of consciousness.
This condition is called presyncope. Presyncope symptoms are:
lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm.
Although sometimes loss of consciousness can occur without any warning signs.
Loss of consciousness is not always caused by syncope. And differential diagnoses always should be made between syncope and other, more serious conditions like: seizures, hypoglycemia, and hypoxemia.
Causes of syncope can be categorized in three main categories:
Vasovagal Syncope; Second; Orthostatic hypotension and Third; Cardiac Syncope.
Vasovagal syncope also called neurally mediated or reflex syncope.
Neurally mediated syncope occurs when blood vessels expand and the heart rate decreases inappropriately.
Such kind of reaction can happen during stress-related situations. Triggers can be: exposure to blood, pain, and strong feelings.
Part of neutally mediated syncope is situational syncope. Such episodes happen during specific situations such as: urination, vomiting and coughing.
Neurally mediated syncope may also occur when an area in the neck known as the carotid sinus is pressed.
Orthostatic hypotension is due to a drop in blood pressure when changing position such as when standing up. It happens because homeostatic reflexes are chronically impaired.
Orthostatic hypotension can be associated with bleeding, dehydration, or significant infection.
Heart-related syncope:
causes may include an abnormal heart rhythm, problems with the heart valves or heart muscle, pulmonary embolism or aortic dissection. This is most serious type of syncope but occurs less often.
Only 10 % of syncopes are caused by cardiac problems.
Ventricular tachycardia can cause syncope, and also can cause death, so, in syncope diagnostic ECG has big role. It can define cardiac causes of syncope.
Supraventricular tachycardia does not cause syncope except in Wolff-Parkinson-White syndrome.
Generally, Syncope is a common condition, around a third of medical students describe at least one syncope in their life.
Risk of syncope increased with age, and its more common among women.
Management of syncope focuses on treating the underlying cause.
Management For neurally mediated syncope is: patient education and avoidance of provocative stimuli.
Intake of fluid and salt is also effective.
Counterpressure maneuvers are effective during the existence of long prodrome, to avoid or delay the onset of syncope.
Such maneuvers include: gripping fingers into a fist, tensing the arms, and crossing the legs or squeezing the thighs together
Recommended acute treatment of vasovagal and orthostatic syncope involves returning blood to the brain by positioning the person on the ground, with legs slightly elevated or sitting leaning forward and the head between the knees for at least 10–15 minutes, preferably in a cool and quiet place.
Characteristics of syncope.
The onset of syncope is rapid, duration is brief and recovery is spontaneous and full.
Syncope is also known as fainting or passing out.
Sometimes some prodromal symptoms occur before loss of consciousness.
This condition is called presyncope. Presyncope symptoms are:
lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm.
Although sometimes loss of consciousness can occur without any warning signs.
Loss of consciousness is not always caused by syncope. And differential diagnoses always should be made between syncope and other, more serious conditions like: seizures, hypoglycemia, and hypoxemia.
Causes of syncope can be categorized in three main categories:
Vasovagal Syncope; Second; Orthostatic hypotension and Third; Cardiac Syncope.
Vasovagal syncope also called neurally mediated or reflex syncope.
Neurally mediated syncope occurs when blood vessels expand and the heart rate decreases inappropriately.
Such kind of reaction can happen during stress-related situations. Triggers can be: exposure to blood, pain, and strong feelings.
Part of neutally mediated syncope is situational syncope. Such episodes happen during specific situations such as: urination, vomiting and coughing.
Neurally mediated syncope may also occur when an area in the neck known as the carotid sinus is pressed.
Orthostatic hypotension is due to a drop in blood pressure when changing position such as when standing up. It happens because homeostatic reflexes are chronically impaired.
Orthostatic hypotension can be associated with bleeding, dehydration, or significant infection.
Heart-related syncope:
causes may include an abnormal heart rhythm, problems with the heart valves or heart muscle, pulmonary embolism or aortic dissection. This is most serious type of syncope but occurs less often.
Only 10 % of syncopes are caused by cardiac problems.
Ventricular tachycardia can cause syncope, and also can cause death, so, in syncope diagnostic ECG has big role. It can define cardiac causes of syncope.
Supraventricular tachycardia does not cause syncope except in Wolff-Parkinson-White syndrome.
Generally, Syncope is a common condition, around a third of medical students describe at least one syncope in their life.
Risk of syncope increased with age, and its more common among women.
Management of syncope focuses on treating the underlying cause.
Management For neurally mediated syncope is: patient education and avoidance of provocative stimuli.
Intake of fluid and salt is also effective.
Counterpressure maneuvers are effective during the existence of long prodrome, to avoid or delay the onset of syncope.
Such maneuvers include: gripping fingers into a fist, tensing the arms, and crossing the legs or squeezing the thighs together
Recommended acute treatment of vasovagal and orthostatic syncope involves returning blood to the brain by positioning the person on the ground, with legs slightly elevated or sitting leaning forward and the head between the knees for at least 10–15 minutes, preferably in a cool and quiet place.
Комментарии
 0:03:51
0:03:51
 0:04:04
0:04:04
 0:05:00
0:05:00
 0:03:29
0:03:29
 0:04:27
0:04:27
 0:01:51
0:01:51
 0:05:29
0:05:29
 0:04:19
0:04:19
 0:05:21
0:05:21
 0:37:05
0:37:05
 0:01:52
0:01:52
 0:06:39
0:06:39
 0:02:43
0:02:43
 0:02:26
0:02:26
 0:06:59
0:06:59
 0:02:11
0:02:11
 0:02:52
0:02:52
 0:24:16
0:24:16
 0:02:16
0:02:16
 0:12:11
0:12:11
 0:25:52
0:25:52
 0:06:06
0:06:06
 0:05:51
0:05:51
 0:03:44
0:03:44