filmov
tv
Randomized Controlled Trials: What it is and how it Reduces Bias

Показать описание
What is a randomized controlled trial (or RCT in short)? This video will share with you the value and key features of RCTs. The best way, or shall I say the gold standard, to assess the effectiveness of most interventions is through an RCT, also referred to as a trial. The design of an RCT is such that the participants or subjects are randomly divided into different groups, most often called the experimental or intervention group and the control group.
Randomization ensures that each group has a fairly similar distribution of known and unknown factors, and reduces confounding factors. If one split participants into, let us say two groups, and we don’t give any intervention to either group, the chances are good that participants will change, for better or for worse. However, if we add an intervention to one group and not to the other while keeping all other factors the same, then the change in the participants’ conditions is most probably due to the intervention provided.
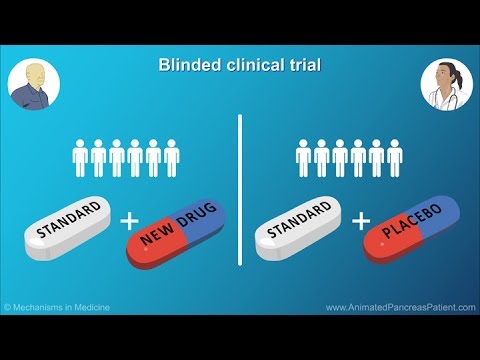
The value of an RCT lies in its scientifically rigorous design. Random and concealed allocation reduces selection bias while blinding of participants and therapists reduces performance bias. Blinding of assessors reduces detection bias. Concealed allocation means that the person allocating the participants to groups either use opaque envelopes which contain the group allocation so that he/she does not know who goes to which groups, or for him/her to be off-site so that he/she is not in contact with the patient and can therefore just send the next randomly allocated number to the study site. If we can create a treatment modality or medication without any active ingredients in it, a placebo treatment, which looks, smells, and tastes exactly like the active treatment, then we’ll be able to blind participants. In areas such as physiotherapy, the social sciences, as well as other areas, it is very difficult not to give away the difference between the active intervention and what is given to the control group. Blinding reduces the placebo or Hawthorne effect.
If the person prescribing the treatment is not being blinded to which group the participants are in, this may lead to unintentional biases in the way in which someone from the control group is approached when the intervention is delivered – from changes in energy, excitement to body language and tone of voice. And the same goes for the intervention group. Again, this is challenging in physiotherapy (and also in other areas) research where we deal with complex interventions. One way around this is to train the therapist to deliver the intervention well so that he/she delivers the intervention in a consistent way.
If the person measuring the outcomes knows who received which treatment, he/she may be biased in assessing the outcome measures. Assessors who are not blinded were known to round up or down numbers that they recorded on their own depending on their own biases.
This video is based on a presentation that was developed for the 2021 World Physiotherapy Congress and I’d like to give a shoutout to my co-presenters Anne Mosely and David Keene.
Randomization ensures that each group has a fairly similar distribution of known and unknown factors, and reduces confounding factors. If one split participants into, let us say two groups, and we don’t give any intervention to either group, the chances are good that participants will change, for better or for worse. However, if we add an intervention to one group and not to the other while keeping all other factors the same, then the change in the participants’ conditions is most probably due to the intervention provided.
The value of an RCT lies in its scientifically rigorous design. Random and concealed allocation reduces selection bias while blinding of participants and therapists reduces performance bias. Blinding of assessors reduces detection bias. Concealed allocation means that the person allocating the participants to groups either use opaque envelopes which contain the group allocation so that he/she does not know who goes to which groups, or for him/her to be off-site so that he/she is not in contact with the patient and can therefore just send the next randomly allocated number to the study site. If we can create a treatment modality or medication without any active ingredients in it, a placebo treatment, which looks, smells, and tastes exactly like the active treatment, then we’ll be able to blind participants. In areas such as physiotherapy, the social sciences, as well as other areas, it is very difficult not to give away the difference between the active intervention and what is given to the control group. Blinding reduces the placebo or Hawthorne effect.
If the person prescribing the treatment is not being blinded to which group the participants are in, this may lead to unintentional biases in the way in which someone from the control group is approached when the intervention is delivered – from changes in energy, excitement to body language and tone of voice. And the same goes for the intervention group. Again, this is challenging in physiotherapy (and also in other areas) research where we deal with complex interventions. One way around this is to train the therapist to deliver the intervention well so that he/she delivers the intervention in a consistent way.
If the person measuring the outcomes knows who received which treatment, he/she may be biased in assessing the outcome measures. Assessors who are not blinded were known to round up or down numbers that they recorded on their own depending on their own biases.
This video is based on a presentation that was developed for the 2021 World Physiotherapy Congress and I’d like to give a shoutout to my co-presenters Anne Mosely and David Keene.
 0:01:55
0:01:55
 0:03:29
0:03:29
 0:03:57
0:03:57
 0:01:30
0:01:30
 0:01:38
0:01:38
 0:52:15
0:52:15
 0:04:50
0:04:50
 0:08:56
0:08:56
 0:35:29
0:35:29
 0:10:01
0:10:01
 0:20:34
0:20:34
 0:05:00
0:05:00
 0:19:12
0:19:12
 0:01:25
0:01:25
 0:07:34
0:07:34
 0:06:39
0:06:39
 0:01:33
0:01:33
 0:03:52
0:03:52
 0:13:57
0:13:57
 0:06:59
0:06:59
 0:08:40
0:08:40
 0:34:39
0:34:39
 0:05:11
0:05:11
 0:08:48
0:08:48