filmov
tv
Osteonecrosis Of The Hip Stages & Treatment - Everything You Need To Know - Dr. Nabil
Показать описание
Dr. Ebraheim’s educational animated video describes osteonecrosis of the femoral head - Hip.
Follow me on twitter:
Osteonecrosis of the Hip
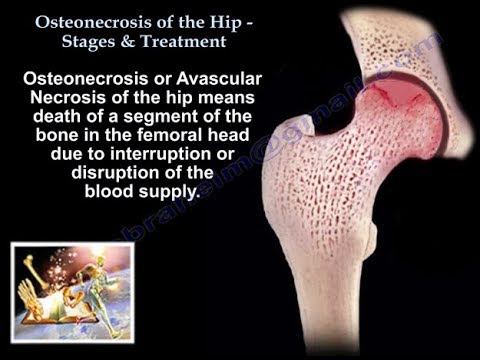
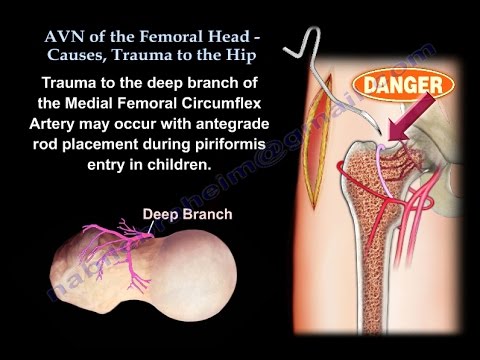
Osteonecrosis or avascular necrosis of the hip means death of a segment of the bone in the femoral head due to interruption of the blood supply. The etiology of this condition is not fully understood. There are several risk factors associated with osteonecrosis of the hip. Direct risk factors for osteonecrosis include trauma, radiation, and hematologic disorders such as lymphoma, leukemia, cytotoxins, Gaucher disease, Caisson disease, and Sickle Cell disease. Indirect risk factors for osteonecrosis include steroid use, alcohol abuse, renal failure, organ transplant, systemic lupus erythematosus (SLE), idiopathic osteonecrosis, hemophilia, and thrombophilia. Osteonecrosis may be bilateral in about 80% of the patients. Check the other hip even if it is asymptomatic. Early diagnosis and treatment may improve the chances for success of a head preserving surgical procedure, such as core decompression or bone grafting. In late stages of osteonecrosis, the femoral head collapses and cannot be saved. For the patient to have a good outcome, the femoral head will need to be replaced at this late stage. Obtain AP and frog leg lateral views of the hip. The frog leg lateral view will show the crescent sign. MRI is the study of choice, especially when the patient has persistent hip pain and the radiographs are negative and the diagnosis of osteonecrosis of the femoral head is suspected, especially if the patient has risk factors. On the T1 MRI, there is a well-defined band of low signal intensity usually within the superior anterior portion of the femoral head. Decreased signal from the ischemic marrow and there is a single band-like area of low signal intensity (crescent sign). The crescent sign represents the reactive interface between the necrotic and reparative zone. The single line density demarcates the normal from the ischemic bone. Double Line Sign is seen in T2 images. The subchondral lesion on T2 shows two lines the low signal intensity line and the high signal intensity line. The lesion will show a high signal intensity inner border with a low signal intensity peripheral rim (double line). The high signal intensity represents hyper vascular granulation tissue. The size of the lesion is the most important factor in determining the development of symptoms and the progression of the disease. The best prognosis occurs in a small lesion with sclerotic margins. The presence of bone marrow edema on the MRI is predictive of worsening of the pain and future progression of the disease. Multifocal osteonecrosis, which is disease involving three or more sites such as the hip, the knee, the shoulder, and the ankle, occurs in about 3% of patients. A patient that presents with osteonecrosis at a site other than the hip should undergo MRI of the hip to rule out the asymptomatic lesion in the femoral head. Transient osteoporosis of the femoral head is not osteonecrosis of the femoral head. In transient osteoporosis, the symptoms are usually more than the x-ray findings. Transient osteoporosis affects pregnant women, and it affects men during the 5th decade of life. On x-ray, you probably will not find much (may find osteopenia). The MRI is probably characteristic (you will find bony edema and increased signal intensity in T2 MRI). The signal changes will involve the femoral head and extend into the neck, and may be even the intertrochanteric area. With transient osteoporosis, there is no double density which is on MRI with osteonecrosis. Transient osteoporosis is not a tumor, it is not osteonecrosis and it does not need surgery. The Ficat classification is a commonly used system to stage osteonecrosis of the hip. Stage I has a normal x-ray; MRI has abnormal signal (changes in the marrow), and the bone scan will show increased uptake. In Stage II, the x-rays will show mixed osteopenia and/or sclerosis. There might be subchondral cysts and lucencies. There is no crescent sign, no subchondral fracture, and no collapse. The MRI and bone scan will be abnormal. In Stage III, the x-ray will show the crescent sign, which is a subchondral fracture line and may be associated with collapse of the femoral head. MRI will show the changes that are seen in the x-rays. In Stage IV, the x-ray will show collapse of the subchondral bone and severe deformity of the head with secondary degenerative changes affecting both sides of the joint.
Follow me on twitter:
Osteonecrosis of the Hip
Osteonecrosis or avascular necrosis of the hip means death of a segment of the bone in the femoral head due to interruption of the blood supply. The etiology of this condition is not fully understood. There are several risk factors associated with osteonecrosis of the hip. Direct risk factors for osteonecrosis include trauma, radiation, and hematologic disorders such as lymphoma, leukemia, cytotoxins, Gaucher disease, Caisson disease, and Sickle Cell disease. Indirect risk factors for osteonecrosis include steroid use, alcohol abuse, renal failure, organ transplant, systemic lupus erythematosus (SLE), idiopathic osteonecrosis, hemophilia, and thrombophilia. Osteonecrosis may be bilateral in about 80% of the patients. Check the other hip even if it is asymptomatic. Early diagnosis and treatment may improve the chances for success of a head preserving surgical procedure, such as core decompression or bone grafting. In late stages of osteonecrosis, the femoral head collapses and cannot be saved. For the patient to have a good outcome, the femoral head will need to be replaced at this late stage. Obtain AP and frog leg lateral views of the hip. The frog leg lateral view will show the crescent sign. MRI is the study of choice, especially when the patient has persistent hip pain and the radiographs are negative and the diagnosis of osteonecrosis of the femoral head is suspected, especially if the patient has risk factors. On the T1 MRI, there is a well-defined band of low signal intensity usually within the superior anterior portion of the femoral head. Decreased signal from the ischemic marrow and there is a single band-like area of low signal intensity (crescent sign). The crescent sign represents the reactive interface between the necrotic and reparative zone. The single line density demarcates the normal from the ischemic bone. Double Line Sign is seen in T2 images. The subchondral lesion on T2 shows two lines the low signal intensity line and the high signal intensity line. The lesion will show a high signal intensity inner border with a low signal intensity peripheral rim (double line). The high signal intensity represents hyper vascular granulation tissue. The size of the lesion is the most important factor in determining the development of symptoms and the progression of the disease. The best prognosis occurs in a small lesion with sclerotic margins. The presence of bone marrow edema on the MRI is predictive of worsening of the pain and future progression of the disease. Multifocal osteonecrosis, which is disease involving three or more sites such as the hip, the knee, the shoulder, and the ankle, occurs in about 3% of patients. A patient that presents with osteonecrosis at a site other than the hip should undergo MRI of the hip to rule out the asymptomatic lesion in the femoral head. Transient osteoporosis of the femoral head is not osteonecrosis of the femoral head. In transient osteoporosis, the symptoms are usually more than the x-ray findings. Transient osteoporosis affects pregnant women, and it affects men during the 5th decade of life. On x-ray, you probably will not find much (may find osteopenia). The MRI is probably characteristic (you will find bony edema and increased signal intensity in T2 MRI). The signal changes will involve the femoral head and extend into the neck, and may be even the intertrochanteric area. With transient osteoporosis, there is no double density which is on MRI with osteonecrosis. Transient osteoporosis is not a tumor, it is not osteonecrosis and it does not need surgery. The Ficat classification is a commonly used system to stage osteonecrosis of the hip. Stage I has a normal x-ray; MRI has abnormal signal (changes in the marrow), and the bone scan will show increased uptake. In Stage II, the x-rays will show mixed osteopenia and/or sclerosis. There might be subchondral cysts and lucencies. There is no crescent sign, no subchondral fracture, and no collapse. The MRI and bone scan will be abnormal. In Stage III, the x-ray will show the crescent sign, which is a subchondral fracture line and may be associated with collapse of the femoral head. MRI will show the changes that are seen in the x-rays. In Stage IV, the x-ray will show collapse of the subchondral bone and severe deformity of the head with secondary degenerative changes affecting both sides of the joint.
Комментарии
 0:03:39
0:03:39
 0:11:28
0:11:28
 0:03:48
0:03:48
 0:04:14
0:04:14
 0:05:11
0:05:11
 0:03:06
0:03:06
 0:07:49
0:07:49
 0:08:01
0:08:01
 0:32:53
0:32:53
 0:01:00
0:01:00
 0:01:00
0:01:00
 0:00:17
0:00:17
 0:04:20
0:04:20
 0:10:17
0:10:17
 0:04:01
0:04:01
 0:01:01
0:01:01
 0:01:00
0:01:00
 0:00:46
0:00:46
 0:01:01
0:01:01
 0:01:57
0:01:57
 0:00:49
0:00:49
 0:02:33
0:02:33
 0:00:26
0:00:26