filmov
tv
Health Care Plans

Показать описание
Employer-sponsored health insurance premium costs rose 203% between 1999 and 2015. Clearly that increase outpaced inflation and workers’ earnings. Deductibles increased during this time also.
There was some good news, however. The cost of family premiums slowed from an average of 11% annual increase to an average of 5%. The cost of family plans (employer and employee parts) ranged from below $10,000 annually to over $24,000 annually.
Health care costs have increased for a variety of reasons. Individuals are living longer and working longer. Whether we like it or not, there is often a correlation between one’s age and the need for health care. And newer medical technologies and newer drugs for treating everything from headaches to cancer are often costly.
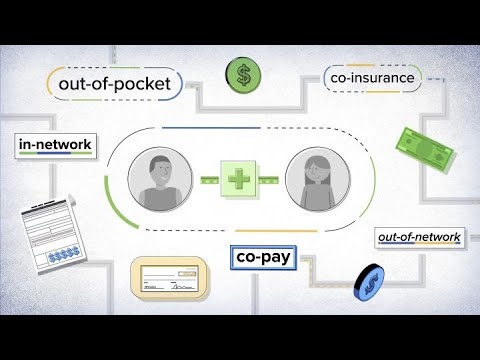
Companies employ a number of different approaches to maintain health care costs. These approaches include traditional plans, managed care, high-deductible health care pro- grams, generic and mail-order drugs, and wellness programs.
Traditional plans include those available through insurance carriers, community-based plans such as Blue Cross/Blue Shield, and employer self-insurance. Managed care plans are the oldest of the approaches to health care cost containment and include health maintenance organizations, preferred provider organizations, and point-of-service plans.
Health maintenance organizations (HMOs), the first type of managed care programs, originated in 1973 when the Health Maintenance Organization Act became law and allowed third-party payers to participate in health care payments. In a PPO, an employer negotiates with health care providers, usually in a network, for discounts.
The third type of plan is a point-of-service plan (POS). This plan can be described as a hybrid of an HMO and a PPO.
In the past several years, more employers have turned to high-deductible health plans (HDHPs) as a way to manage the costs of employee health care plans. HDHPs are also referred to as catastrophic health plans because they don’t pay for the first few thousand dollars of a person’s medical costs each year.
HSAs are an example of an Account-Based Health Plan (ABHP), a consumer-driven plan that pairs a group health plan with a tax-advantaged medical spending account. HSAs provide a way for employees to pay for their immediate health care expenses not covered by an HDHP and save money on a tax-free basis.
Instead of contracting with an insurer such as Blue Cross/ Blue Shield or Cigna to design and deliver all or part of their benefits programs, companies can decide to self-fund their programs (self-insure). Many large employers and a growing number of medium and small employers make this decision each year. By self-funding, employers avoid having to pay premiums and taxes on those premiums, and they avoid some of the state requirements for benefits.
There was some good news, however. The cost of family premiums slowed from an average of 11% annual increase to an average of 5%. The cost of family plans (employer and employee parts) ranged from below $10,000 annually to over $24,000 annually.
Health care costs have increased for a variety of reasons. Individuals are living longer and working longer. Whether we like it or not, there is often a correlation between one’s age and the need for health care. And newer medical technologies and newer drugs for treating everything from headaches to cancer are often costly.
Companies employ a number of different approaches to maintain health care costs. These approaches include traditional plans, managed care, high-deductible health care pro- grams, generic and mail-order drugs, and wellness programs.
Traditional plans include those available through insurance carriers, community-based plans such as Blue Cross/Blue Shield, and employer self-insurance. Managed care plans are the oldest of the approaches to health care cost containment and include health maintenance organizations, preferred provider organizations, and point-of-service plans.
Health maintenance organizations (HMOs), the first type of managed care programs, originated in 1973 when the Health Maintenance Organization Act became law and allowed third-party payers to participate in health care payments. In a PPO, an employer negotiates with health care providers, usually in a network, for discounts.
The third type of plan is a point-of-service plan (POS). This plan can be described as a hybrid of an HMO and a PPO.
In the past several years, more employers have turned to high-deductible health plans (HDHPs) as a way to manage the costs of employee health care plans. HDHPs are also referred to as catastrophic health plans because they don’t pay for the first few thousand dollars of a person’s medical costs each year.
HSAs are an example of an Account-Based Health Plan (ABHP), a consumer-driven plan that pairs a group health plan with a tax-advantaged medical spending account. HSAs provide a way for employees to pay for their immediate health care expenses not covered by an HDHP and save money on a tax-free basis.
Instead of contracting with an insurer such as Blue Cross/ Blue Shield or Cigna to design and deliver all or part of their benefits programs, companies can decide to self-fund their programs (self-insure). Many large employers and a growing number of medium and small employers make this decision each year. By self-funding, employers avoid having to pay premiums and taxes on those premiums, and they avoid some of the state requirements for benefits.
Комментарии
 0:03:00
0:03:00
 0:14:13
0:14:13
 0:02:33
0:02:33
 0:04:55
0:04:55
 0:06:07
0:06:07
 0:09:57
0:09:57
 0:04:29
0:04:29
 0:03:11
0:03:11
 0:24:12
0:24:12
 0:00:53
0:00:53
 0:07:04
0:07:04
 0:01:09
0:01:09
 0:03:57
0:03:57
 0:04:37
0:04:37
 0:06:41
0:06:41
 0:03:16
0:03:16
 0:15:23
0:15:23
 0:01:03
0:01:03
 0:06:55
0:06:55
 0:00:22
0:00:22
 0:01:46
0:01:46
 0:02:00
0:02:00
 0:08:07
0:08:07
 0:05:50
0:05:50