filmov
tv
Autoimmune Encephalitis: What Psychiatrists Need to Know

Показать описание
Dr. Pojen Deng completed his medical degree from the Warren Alpert Medical School of Brown University. He then completed dual residency training in neurology and psychiatry at the NYU Medical Center. He joined the Mount Sinai Health System as a neurohospitalist with additional outpatient practice in neuropsychiatry, where he treats conditions at the interface of neurology and psychiatry with particular interests in neuroimmunology and epilepsy. His Clinical focus is on Encephalitis, Epilepsy, Cognitive impairment with a research focus on Inflammation, Psychiatry.
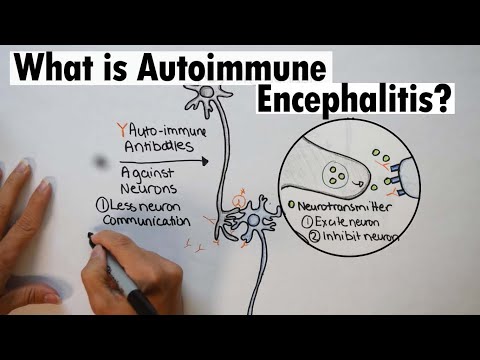
When you got sick, did you have psychiatric symptoms? Psychosis, hallucinations, paranoia? (to name a few). Where you misdiagnosed? Put on a psych hold? Did they think you had Bipolar disorder or schizophrenia? Some patients have even been accused of drug abuse without evidence. The onset of autoimmune encephalitis can look like any of these. It’s a challenging diagnosis to make and often psychiatrists see us first. Therefore, it is extremely important for psychiatrist to be able to identify when the patient might be suffering from AE and call in neurology for a full work up including a lumbar puncture.
Dr. Deng’s presentation gives an overview of limbic encephalitis and what occurs in the disease process that creates these neuropsychiatric symptoms and outlines the red flags psychiatrists, clinicians and laypeople should be aware of that would indicate autoimmune encephalitis could be the culprit to first episode of psychosis (FEP). One of the diagnostic challenges that happens in autoimmune encephalitis is that demographically it often maps directly on the age ranges of first break psychosis. A sensitive and common issue is that many doctors, patients and families are led to view psychiatric illness and encephalitis as mutually exclusive issues, when the reality is that encephalitis very much includes psychiatric illness and requires psychiatric treatment, in addition to neurologic treatment. Many families and patients experience delays in care or, even inappropriate care. Ideally, these two specialties should be working in tandem with the emphasis that both neurologic care and psychiatric care occurs with all autoimmune encephalitis patients.
The International Autoimmune Encephalitis Society, (IAES), is the only Family/Patient-centered organization for people with a diagnosis of Autoimmune Encephalitis. Leading with integrity, IAES strives to advance services, education, increased awareness and research for this group of diseases. IAES provides science-based information backed by trusted medical experts in the field of autoimmune neurology and relies on the expertise of our Medical Advisory Board. We are an established non-profit organization with a history of supporting all-inclusive services from diagnosis to recovery and the many challenges experienced in that journey.
Welcome to our ‘AE Family’, the family you never knew you had.
Your donations help us continue our important work.
When you got sick, did you have psychiatric symptoms? Psychosis, hallucinations, paranoia? (to name a few). Where you misdiagnosed? Put on a psych hold? Did they think you had Bipolar disorder or schizophrenia? Some patients have even been accused of drug abuse without evidence. The onset of autoimmune encephalitis can look like any of these. It’s a challenging diagnosis to make and often psychiatrists see us first. Therefore, it is extremely important for psychiatrist to be able to identify when the patient might be suffering from AE and call in neurology for a full work up including a lumbar puncture.
Dr. Deng’s presentation gives an overview of limbic encephalitis and what occurs in the disease process that creates these neuropsychiatric symptoms and outlines the red flags psychiatrists, clinicians and laypeople should be aware of that would indicate autoimmune encephalitis could be the culprit to first episode of psychosis (FEP). One of the diagnostic challenges that happens in autoimmune encephalitis is that demographically it often maps directly on the age ranges of first break psychosis. A sensitive and common issue is that many doctors, patients and families are led to view psychiatric illness and encephalitis as mutually exclusive issues, when the reality is that encephalitis very much includes psychiatric illness and requires psychiatric treatment, in addition to neurologic treatment. Many families and patients experience delays in care or, even inappropriate care. Ideally, these two specialties should be working in tandem with the emphasis that both neurologic care and psychiatric care occurs with all autoimmune encephalitis patients.
The International Autoimmune Encephalitis Society, (IAES), is the only Family/Patient-centered organization for people with a diagnosis of Autoimmune Encephalitis. Leading with integrity, IAES strives to advance services, education, increased awareness and research for this group of diseases. IAES provides science-based information backed by trusted medical experts in the field of autoimmune neurology and relies on the expertise of our Medical Advisory Board. We are an established non-profit organization with a history of supporting all-inclusive services from diagnosis to recovery and the many challenges experienced in that journey.
Welcome to our ‘AE Family’, the family you never knew you had.
Your donations help us continue our important work.
 1:06:50
1:06:50
 0:58:53
0:58:53
 0:25:21
0:25:21
 0:04:54
0:04:54
 0:29:48
0:29:48
 0:14:26
0:14:26
 0:04:03
0:04:03
 0:30:31
0:30:31
 1:09:03
1:09:03
 0:24:43
0:24:43
 0:28:13
0:28:13
 0:24:12
0:24:12
 0:51:15
0:51:15
 0:12:11
0:12:11
 0:10:08
0:10:08
 0:58:35
0:58:35
 1:07:09
1:07:09
 1:02:43
1:02:43
 0:02:08
0:02:08
 0:44:31
0:44:31
 0:28:13
0:28:13
 0:02:17
0:02:17
 0:19:32
0:19:32
 0:13:53
0:13:53