filmov
tv
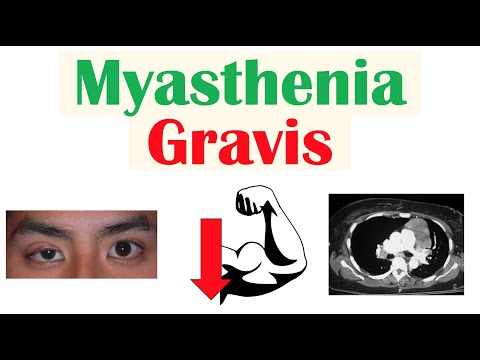
Myasthenia gravis is a big deal to anesthesiologists

Показать описание
Myasthenia gravis is a disease that literally means "grave muscle weakness" and it has serious implications for anesthetic care. In this video, I explain why myasthenia gravis gets special attention from anesthesiologists, and how it can change anesthetic management.
0:00 Start
0:59 Myasthenia gravis
2:35 Paralysis in anesthesia
3:57 MG & paralytics
5:12 Reversal agents
6:07 Avoiding paralytics?
Music:
The information in this video is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional.
#Anesthesiology #Residency #MedicalSchool
0:00 Start
0:59 Myasthenia gravis
2:35 Paralysis in anesthesia
3:57 MG & paralytics
5:12 Reversal agents
6:07 Avoiding paralytics?
Music:
The information in this video is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional.
#Anesthesiology #Residency #MedicalSchool
Myasthenia gravis is a big deal to anesthesiologists
Myasthenia Gravis
Myasthenia Gravis - symptoms, pathophysiology, investigations, treatment
Understanding Myasthenia Gravis: Diagnosis and Treatment Options Explained by Dr. David Saperstein
Diagnostic Delays are Common for Myasthenia Gravis Patients
I Have Seronegative Myasthenia Gravis
Myastenia Gravis explained!
Greg's Story Living with Myasthenia Gravis - gMG Never Rests
Current State of Treating, Managing Myasthenia Gravis
Myasthenia Gravis | Pathophysiology, Signs & Symptoms, Diagnosis, Treatment
Myasthenia Gravis Remission with Vitamin D
Behind the Mystery: Myasthenia Gravis
Myasthenia Gravis: Patient Perspective and the Current Disease State
What is Myasthenia Gravis | All you need to know | Causes | Symptoms | Diagnosis | Treatment
The Basics of Myasthenia Gravis: Symptoms, Causes, Treatments
What Causes MYASTHENIA GRAVIS? // Autoimmune Pathophysiology – Med-Surg Nursing | Lecturio
Myasthenia Gravis
What is Myasthenia Gravis(Muscular Disorder) | Big Apollo Spectra Hospital, Patna
Role of Thymectomy in Myasthenia Gravis Treatment - Dr. (Prof.) Arvind Kumar, Medanta +919773635888
OPEN Monday I Living with Myasthenia Gravis
Myasthenia Gravis
MYASTHENIA GRAVIS Explained by Dr. Stephen Cabral
Novel Therapies in AChR + Myasthenia Gravis
MYASTHENIA GRAVIS: My Diagnosis Story!
Комментарии
 0:08:04
0:08:04
 0:36:32
0:36:32
 0:13:55
0:13:55
 0:40:11
0:40:11
 0:02:15
0:02:15
 0:06:36
0:06:36
 0:01:01
0:01:01
 0:05:31
0:05:31
 0:08:48
0:08:48
 0:13:18
0:13:18
 0:04:04
0:04:04
 0:09:32
0:09:32
 0:14:39
0:14:39
 0:12:55
0:12:55
 0:13:48
0:13:48
 0:04:52
0:04:52
 0:15:33
0:15:33
 0:05:26
0:05:26
 0:02:45
0:02:45
 0:08:03
0:08:03
 0:20:54
0:20:54
 0:02:36
0:02:36
 0:39:08
0:39:08
 0:07:35
0:07:35