filmov
tv
Restrictive Lung Diseases | Clinical Medicine

Показать описание
Ninja Nerds!
Professor Zach Murphy will be presenting on Restrictive Lung Disease. We will be going into detail on the following main objectives:
1. Definition and Classification of Restrictive Lung Disease
- Gain insights into what constitutes restrictive lung disease and how it varies from obstructive lung conditions.
- Acquaint yourself with the classifications based on etiology, such as intrinsic lung diseases (interstitial lung disease, fibrosis) and extrinsic factors (pleural diseases, neuromuscular disorders).
2. Pathophysiology and Etiologies
- Explore the underlying mechanisms contributing to restrictive lung disease, ranging from inflammation and fibrosis to pleural effusions and chest wall deformities.
- Understand the altered lung mechanics and its relationship to the various causative factors.
3. Clinical Manifestations and Presentation
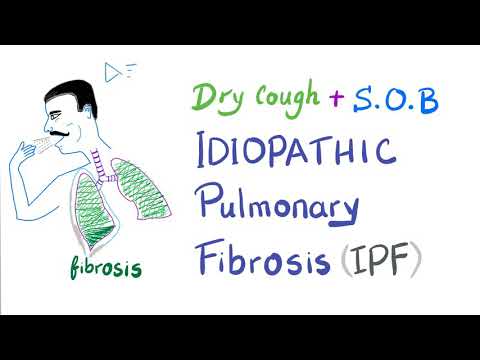
- Learn to recognize the signs and symptoms commonly associated with restrictive lung disease, such as dyspnea, reduced exercise tolerance, and dry cough.
- Identify potential indicators of severity, such as hypoxia, tachypnea, and the use of accessory respiratory muscles.
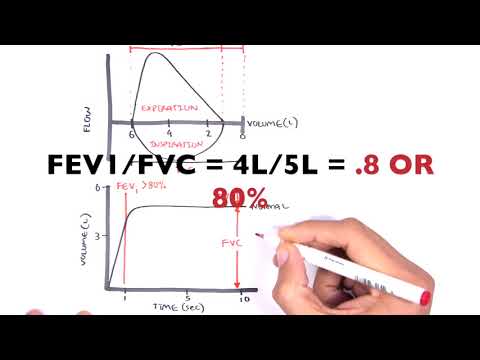
4. Diagnostic Criteria and Tools
- Understand the roles and interpretations of various diagnostic tests, including pulmonary function tests (PFTs), high-resolution computed tomography (HRCT), and lung biopsy.
- Familiarize yourself with the latest guidelines for diagnosing restrictive lung disease as outlined by professional bodies like the American Thoracic Society.
5. Initial Management Strategies
- Discuss evidence-based approaches for initial symptom management, such as oxygen supplementation and corticosteroids.
- Learn about the importance of supportive therapies, including physiotherapy and pulmonary rehabilitation, in enhancing quality of life.
6. Definitive Management Approaches
- Examine the various treatment options available, ranging from pharmacological interventions like antifibrotic agents to surgical procedures like lung transplantation.
- Evaluate the risks and benefits of each approach, grounded in the latest research and guidelines.
7. Complications and Prognosis
- Gain an understanding of the potential complications arising from untreated or improperly managed restrictive lung disease, such as respiratory failure and pulmonary hypertension.
- Discuss the prognostic indicators and how variables like age, lung function, and comorbidities may influence outcomes.
Table of Contents:
0:00 Lab
0:07 Restrictive Lung Disease Introduction
0:37 Pathophysiology | Intrinsic Lung Diseases
8:07 Pathophysiology | Extrinsic Lung Diseases
11:45 Complications | Respiratory Failure
15:52 Complications | Cor Pulmonale
19:42 Complications | Lung Cancer
21:55 Diagnostic Approach
27:11 Treatment
29:29 Comment, Like, SUBSCRIBE!
Retired Ninja Nerd Lectures:
#ninjanerd #respiratory #restrictivelungdiseases
Комментарии
 0:29:50
0:29:50
 0:17:28
0:17:28
 0:11:40
0:11:40
 0:16:50
0:16:50
 0:05:08
0:05:08
 0:24:26
0:24:26
 0:09:33
0:09:33
 0:14:39
0:14:39
 0:09:58
0:09:58
 0:16:33
0:16:33
 0:10:09
0:10:09
 0:14:12
0:14:12
 0:46:22
0:46:22
 0:16:18
0:16:18
 0:04:49
0:04:49
 0:04:09
0:04:09
 0:04:18
0:04:18
 0:11:01
0:11:01
 0:12:20
0:12:20
 0:01:51
0:01:51
 1:25:51
1:25:51
 0:13:53
0:13:53
 0:10:41
0:10:41
 0:22:31
0:22:31