filmov
tv
The challenges of preventing ICU delirium with patients in isolation

Показать описание
Part of Philips patient monitoring educational series about supporting care of patients with COVID-19, this webinar provides information about the challenges associated with ICU delirium in patient in isolation.
The challenges of preventing ICU delirium with patients in isolation
Why a stay in the ICU can leave patients worse off
A Clinical Psychologist Talks About the Challenges Inside and After the ICU for COVID-19 Patients
CASE STUDY: HOW TO STOP THE ICU TEAM FROM WITHDRAWING LIFE SUPPORT WITHOUT FAMILY CONSENT!
How an ICU works to prevent or treat hospital-acquired infections.
Prevention of ICU over-crowding following CAR-T
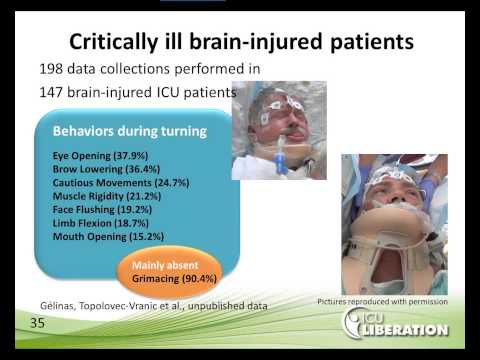
ICU Liberation: Successfully Overcoming Assessment and Treatment Challenges for ICU Pain
ICS Education: Managing the COVID-ICU Surge
Emergency Q&A for Families in ICU and INTENSIVE CARE AT HOME!
Innovative Infection Control Strategies in the ICU
Antimicrobial Stewardship In ICU Setting: Challenges And Solutions
The ICU Experience: What to Expect and How to Cope #ICU #cancertreatment #cancerfax
Strategies for Assessing Pain in the ICU
Webinar: Navigating Nutrition Challenges in ICU Patients: A Case-Based Panel Discussion (2024)
A day with me as an icu nurse in hospital 🏥 #nurse #hospital #icu #dailyvlog
Nurse Monica vs. 9 Ventilated Patients: The Ultimate ICU Challenge!
Rebuilding What We've Lost in Covid: A Perspective from the ICU
An Integrated Approach to ICU Delirium Assessment, Prevention and Management
ICU Keeps Telling Me that They Can't Take My Loved One Off the Ventilator Due to Agitation! Hel...
A day in ICU for a nurse #shorts
Addressing Patient Comfort issue in the ICU ! (3min)
The Hidden Struggles of ICU Survivors: Mental Health Perspectives and Therapeutic Strategies
Preventing disabling muscle loss in ICU survivors - St. Michael's Angels' Den
𝐏𝐎𝐖𝐄𝐑 𝐎𝐅 𝐂𝐎𝐍𝐍𝐄𝐂𝐓𝐄𝐃 𝐂𝐀𝐑𝐄 𝐈𝐍 𝐈𝐂𝐔’𝐬...
Комментарии
 0:43:55
0:43:55
 0:07:50
0:07:50
 0:13:40
0:13:40
 0:00:56
0:00:56
 0:02:00
0:02:00
 0:01:33
0:01:33
 0:59:10
0:59:10
 0:58:24
0:58:24
 1:00:59
1:00:59
 0:27:28
0:27:28
 0:57:15
0:57:15
 0:00:11
0:00:11
 0:19:39
0:19:39
 1:03:16
1:03:16
 0:00:16
0:00:16
 0:00:06
0:00:06
 0:59:24
0:59:24
 0:59:09
0:59:09
 0:00:58
0:00:58
 0:00:16
0:00:16
 0:03:03
0:03:03
 1:03:48
1:03:48
 0:03:04
0:03:04
 1:05:45
1:05:45