filmov
tv
AngiotensinII vsNorepinephrine Impact on Pulmonary Vascular Resistance in Cardiac#pencis #cardiology

Показать описание
Angiotensin II vs. Norepinephrine: Impact on Pulmonary Vascular Resistance in Cardiac Surgery
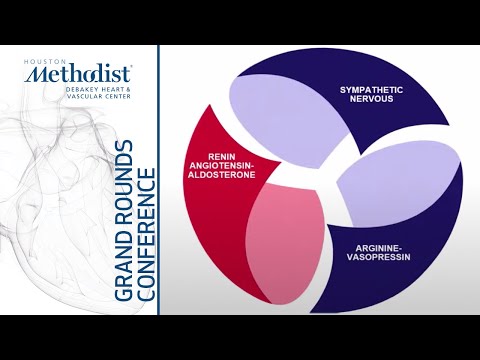
Pulmonary vascular resistance (PVR) is an important factor in managing patients undergoing cardiac surgery, particularly in those with heart failure or pulmonary hypertension. Both Angiotensin II and Norepinephrine are commonly used vasopressors to stabilize blood pressure during surgery. However, they affect PVR differently:
Angiotensin II is a potent vasoconstrictor that works by stimulating the renin-angiotensin system, which can increase systemic vascular resistance and blood pressure. Its impact on pulmonary circulation is less pronounced, potentially making it a favorable choice in patients where excessive pulmonary vasoconstriction would be undesirable.
Norepinephrine, another powerful vasoconstrictor, primarily acts on alpha-adrenergic receptors. It increases systemic blood pressure and can also increase PVR, which may exacerbate right ventricular load in patients with pulmonary hypertension. This makes its use in such scenarios more cautious.
In cardiac surgery, particularly during or after procedures like coronary artery bypass grafting (CABG) or valve replacement, the balance between these agents is critical. Managing PVR is essential for preventing right heart failure and maintaining optimal oxygenation. Studies suggest that Angiotensin II may have a more favorable profile for patients with elevated PVR, as it tends to have a lesser effect on pulmonary circulation compared to norepinephrine.
#CardiacSurgery
#PulmonaryHypertension
#AngiotensinII
#Norepinephrine
#PulmonaryVascularResistance
#HeartFailure
#Vasopressors
#RightHeartFailure
#CardiovascularResearch
#CABGSurgery
#HeartHealth
#CardioCare
Pulmonary vascular resistance (PVR) is an important factor in managing patients undergoing cardiac surgery, particularly in those with heart failure or pulmonary hypertension. Both Angiotensin II and Norepinephrine are commonly used vasopressors to stabilize blood pressure during surgery. However, they affect PVR differently:
Angiotensin II is a potent vasoconstrictor that works by stimulating the renin-angiotensin system, which can increase systemic vascular resistance and blood pressure. Its impact on pulmonary circulation is less pronounced, potentially making it a favorable choice in patients where excessive pulmonary vasoconstriction would be undesirable.
Norepinephrine, another powerful vasoconstrictor, primarily acts on alpha-adrenergic receptors. It increases systemic blood pressure and can also increase PVR, which may exacerbate right ventricular load in patients with pulmonary hypertension. This makes its use in such scenarios more cautious.
In cardiac surgery, particularly during or after procedures like coronary artery bypass grafting (CABG) or valve replacement, the balance between these agents is critical. Managing PVR is essential for preventing right heart failure and maintaining optimal oxygenation. Studies suggest that Angiotensin II may have a more favorable profile for patients with elevated PVR, as it tends to have a lesser effect on pulmonary circulation compared to norepinephrine.
#CardiacSurgery
#PulmonaryHypertension
#AngiotensinII
#Norepinephrine
#PulmonaryVascularResistance
#HeartFailure
#Vasopressors
#RightHeartFailure
#CardiovascularResearch
#CABGSurgery
#HeartHealth
#CardioCare
 0:01:00
0:01:00
 0:23:48
0:23:48
 1:26:26
1:26:26
 0:08:31
0:08:31
 0:17:05
0:17:05
 0:01:31
0:01:31
 0:17:40
0:17:40
 0:17:17
0:17:17
![Pharmacology [ANS] 14-](https://i.ytimg.com/vi/pecBsjQdMzc/hqdefault.jpg) 0:10:17
0:10:17
 0:56:59
0:56:59
 0:38:38
0:38:38
 1:17:13
1:17:13
 0:22:58
0:22:58
 0:26:46
0:26:46
 0:52:54
0:52:54
 1:42:39
1:42:39
 0:48:02
0:48:02
 0:58:03
0:58:03
 1:25:02
1:25:02