filmov
tv
Katskee v. Blue Cross/Blue Shield of Nebraska Case Brief Summary | Law Case Explained

Показать описание
Katskee v. Blue Cross/Blue Shield of Nebraska | 515 N.W.2d 645 (1994)
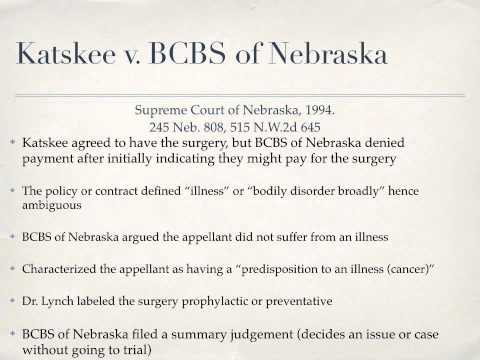
Generally, an insurance company’s liability to pay for an insured’s medical payments under an insurance policy depends on how the policy’s language is construed. Although certain terms aren’t ambiguous and susceptible to different interpretations, other terms are ambiguous and may require a court to ascertain the parties’ intent. In Katskee versus Blue Cross Blue Shield of Nebraska, the Nebraska Supreme Court considered whether the terms bodily disorder and disease used in an insurance policy to define the word illness were ambiguous.
In January of nineteen ninety, based on her gynecologist’s recommendation, Sindie Katskee consulted with Doctor Henry Lynch about her family’s history of breast and ovarian cancer. After an examination, Lynch diagnosed Katskee with breast-ovarian carcinoma syndrome. Lynch also recommended that Katskee have surgery to remove her uterus, ovaries, and fallopian tubes.
Although Katskee’s diagnosis put her at a high risk of developing cancer, Katskee didn’t have cancer.
After considering her options, Katskee decided to have the surgery. Prior to the procedure, she filed a claim with her insurance provider, Blue Cross Blue Shield of Nebraska, which we’ll call Blue Cross. In addition, Lynch and Katskee’s gynecologist wrote letters to Blue Cross on Katskee’s behalf explaining why the operation was necessary.
Initially, Blue Cross told Katskee that it might pay for her surgery. However, two weeks before surgery, Doctor Roger Mason, Blue Cross’s chief medical officer, sent a letter to Katskee informing her that the insurer wouldn’t cover the surgery’s cost. Specifically, Mason stated that the surgery wasn’t medically necessary and wasn’t covered under Katskee’s insurance policy.
After the operation, Katskee sued Blue Cross in state district court for breach of contract, seeking to recover the costs of the operation. In response, Blue Cross moved for summary judgment. In granting Blue Cross’s motion, the court concluded three things. First, Katskee’s condition wasn’t covered by the policy. Second, Katskee didn’t have an illness covered by the policy. And third, Blue Cross had the right to determine what was medically necessary under the policy. Katskee appealed to the court of appeals, and the case was removed to the Nebraska Supreme Court.
#casebriefs #lawcases #casesummaries
 0:02:44
0:02:44
 0:01:30
0:01:30
 0:00:31
0:00:31
 0:24:25
0:24:25
 0:01:53
0:01:53
 0:28:12
0:28:12
 0:01:26
0:01:26
 0:02:19
0:02:19
 0:01:57
0:01:57
 0:02:03
0:02:03
 0:02:46
0:02:46
 0:02:25
0:02:25
 0:18:49
0:18:49
 0:29:33
0:29:33