filmov
tv
Incidental pancreatic cysts - what we know and what we don't know, Jay Heiken

Показать описание
Pancreatic cysts are very common in the adult population, and the prevalence increases with age. Pancreatic cysts are identified in 13%-20% of adults undergoing abdominal magnetic resonance imaging (MRI) [1, 2] and in 2.6% of individuals undergoing multi-detector CT [3]. How we deal with these cystic lesions has important implications for both patient care and the expenditure of healthcare dollars.
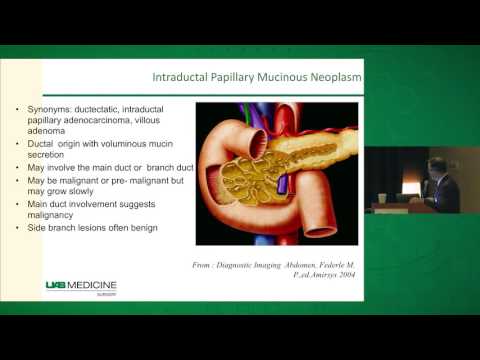
Most pancreatic cysts discovered incidentally on imaging studies are branch duct intraductal papillary mucinous neoplasms (BD-IPMN). The vast majority are larger than 3cm and have a very low risk of malignancy [4]. Nevertheless, certain imaging features of pancreatic cysts are associated with an increased risk of malignancy. The international consensus guidelines for the management of pancreatic mucinous neoplasms [4] identify a group of features which are characterized as “worrisome features” (size larger or equal to 3 cm, thickened enhanced wall, main pancreatic duct (MPD) size 5-9 mm, non-enhanced mural nodule(s), abrupt change in MPD caliber with atrophy of the upstream pancreas, and lymphadenopathy) and “high-risk stigmata” (obstructive jaundice in a patient with a pancreatic head lesion, enhanced solid component, and MPD size larger or equal to 10 mm).
Recent surgical data indicate that individuals with pancreatic cysts may be at increased risk of developing solid pancreatic neoplasms. 4%-10% of patients with resected BD-IPMN are found to have concurrent pancreatic ductal adenocarcinoma [5, 6]. In addition, patients with one or more pancreatic cysts have an increased risk of subsequent development of pancreatic ductal adenocarcinoma [7, 8].
Whether individuals with multifocal BD-IPMN are at increased risk of malignancy is unclear. Although most studies have not shown an increased risk of malignancy compared with solitary BD-IPMN, on study found that in 52 patients with larger or equal to 4 pancreatic cysts, 34% had high grade dysplasia or invasive carcinoma and 17% had a coexistent ductal adenocarcinoma [9].
Almost all of the data available on the biological behavior of pancreatic cysts come from surgical series and longitudinal imaging studies. No randomised controlled trials have been performed. Therefore our approach to the management of incidentally discovered pancreatic cysts is based on consensus guidelines developed by panels of medicine, surgery, pathology and imaging experts [4, 10, 11], and there is still a great deal to be learned about the genetics, natural history and risks associated with these cysts.
All of the consensus guidelines recommend that a cyst larger or equal to 3 cm should be followed as long as it contains no worrisome or high-risk features; however, what the follow-up schedule should be and when surgical intervention is indicated varies among the guidelines. Most consensus panels indicate that endoscopic ultrasound (EUS) with cyst aspiration should be considered to try to characterise cysts larger or equal to 2 cm.
It is important to bear in mind that the appearance of a pancreatic cyst on an imaging study does not translate directly into patient management. Appropriate management of an individual with an incidentally discovered pancreatic cyst depends upon multiple factors including age, comorbidities, the individual’s willingness to undergo surveillance or surgery, and family history of pancreatic cancer. Therefore management decisions should be individualised and based on multidisciplinary team discussion.
References
Комментарии
 0:23:04
0:23:04
 0:17:44
0:17:44
 0:02:57
0:02:57
 0:09:48
0:09:48
 0:17:27
0:17:27
 0:14:38
0:14:38
 0:07:10
0:07:10
 0:02:45
0:02:45
 0:21:44
0:21:44
 0:07:01
0:07:01
 0:04:03
0:04:03
 0:02:43
0:02:43
 0:03:17
0:03:17
 0:03:07
0:03:07
 1:08:02
1:08:02
 0:29:10
0:29:10
 0:03:04
0:03:04
 0:48:23
0:48:23
 0:20:42
0:20:42
 0:36:12
0:36:12
 0:48:23
0:48:23
 0:19:00
0:19:00
 1:06:01
1:06:01
 0:16:59
0:16:59