filmov
tv
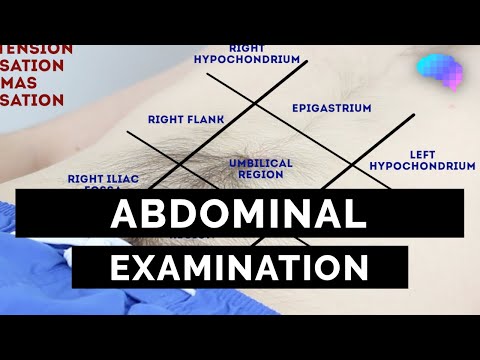
Abdominal Examination, Demonstration of all steps, Part 1

Показать описание
An abdominal examination is a physical examination of the abdomen, typically involving inspection, auscultation, palpation, and percussion, to assess for signs of disease or abnormalities in the abdominal organs and surrounding tissues.
Here's a more detailed breakdown:
1. Preparation:
Positioning:
The patient should be positioned supine (lying on their back) with knees slightly bent and arms at their sides.
Expose the abdomen:
Adequately expose the abdomen from the waist up, while maintaining patient privacy.
Good lighting:
Ensure adequate lighting for proper inspection.
Warm hands and stethoscope:
Use a pre-warmed stethoscope and ensure your hands are warm to avoid startling the patient.
2. Examination Techniques:
Inspection:
General appearance: Observe the overall appearance of the abdomen, noting any signs of distension, masses, or asymmetry.
Skin: Look for scars, striae, rashes, or discoloration.
Umbilicus: Inspect the umbilicus for any abnormalities.
Movement: Observe for any pulsations or peristaltic waves.
Auscultation:
Bowel sounds: Listen for bowel sounds in all four quadrants, noting their frequency, character, and presence of any abnormal sounds like borborygmi (rumbling sounds).
Vascular sounds: Listen for bruits (abnormal sounds) over the abdominal aorta and renal arteries.
Palpation:
Light palpation: Gently palpate the abdomen to assess for tenderness, masses, or guarding (tensing of the abdominal muscles).
Deep palpation: Palpate deeper to assess for organomegaly (enlarged organs), masses, or tenderness.
Specific organ palpation: Palpate for the liver, spleen, kidneys, and other organs as needed.
Percussion:
General percussion: Percuss the abdomen to assess for fluid, gas, or masses.
Percussion of specific organs: Percuss the liver and spleen to assess their size and position.
3. Key Areas to Assess:
Suprapubic area: Palpate for a distended bladder.
Umbilical area: Palpate for masses or pulsations.
Flanks: Palpate for kidney masses or tenderness.
Lower quadrants: Palpate for masses or tenderness.
4. Special Tests:
Shifting dullness:
Test for ascites (fluid in the abdominal cavity) by percussing the abdomen and noting any shifting dullness.
Rebound tenderness:
Assess for peritoneal irritation by gently palpating the abdomen and then rapidly releasing your fingers.
Guarding:
Assess for guarding (tensing of the abdominal muscles) by palpating the abdomen.
5. Documentation:
Record your findings:
Document all your findings in a clear and concise manner, including any abnormalities or tenderness.
Include patient history:
Include relevant patient history, such as any past abdominal surgeries or symptoms.
Here's a more detailed breakdown:
1. Preparation:
Positioning:
The patient should be positioned supine (lying on their back) with knees slightly bent and arms at their sides.
Expose the abdomen:
Adequately expose the abdomen from the waist up, while maintaining patient privacy.
Good lighting:
Ensure adequate lighting for proper inspection.
Warm hands and stethoscope:
Use a pre-warmed stethoscope and ensure your hands are warm to avoid startling the patient.
2. Examination Techniques:
Inspection:
General appearance: Observe the overall appearance of the abdomen, noting any signs of distension, masses, or asymmetry.
Skin: Look for scars, striae, rashes, or discoloration.
Umbilicus: Inspect the umbilicus for any abnormalities.
Movement: Observe for any pulsations or peristaltic waves.
Auscultation:
Bowel sounds: Listen for bowel sounds in all four quadrants, noting their frequency, character, and presence of any abnormal sounds like borborygmi (rumbling sounds).
Vascular sounds: Listen for bruits (abnormal sounds) over the abdominal aorta and renal arteries.
Palpation:
Light palpation: Gently palpate the abdomen to assess for tenderness, masses, or guarding (tensing of the abdominal muscles).
Deep palpation: Palpate deeper to assess for organomegaly (enlarged organs), masses, or tenderness.
Specific organ palpation: Palpate for the liver, spleen, kidneys, and other organs as needed.
Percussion:
General percussion: Percuss the abdomen to assess for fluid, gas, or masses.
Percussion of specific organs: Percuss the liver and spleen to assess their size and position.
3. Key Areas to Assess:
Suprapubic area: Palpate for a distended bladder.
Umbilical area: Palpate for masses or pulsations.
Flanks: Palpate for kidney masses or tenderness.
Lower quadrants: Palpate for masses or tenderness.
4. Special Tests:
Shifting dullness:
Test for ascites (fluid in the abdominal cavity) by percussing the abdomen and noting any shifting dullness.
Rebound tenderness:
Assess for peritoneal irritation by gently palpating the abdomen and then rapidly releasing your fingers.
Guarding:
Assess for guarding (tensing of the abdominal muscles) by palpating the abdomen.
5. Documentation:
Record your findings:
Document all your findings in a clear and concise manner, including any abnormalities or tenderness.
Include patient history:
Include relevant patient history, such as any past abdominal surgeries or symptoms.
 0:08:22
0:08:22
 0:12:47
0:12:47
 0:02:00
0:02:00
 0:08:11
0:08:11
 0:09:47
0:09:47
 0:02:16
0:02:16
 0:12:04
0:12:04
 0:00:58
0:00:58
 0:10:04
0:10:04
 0:05:00
0:05:00
 0:31:10
0:31:10
 0:00:27
0:00:27
 0:07:26
0:07:26
 0:12:31
0:12:31
 0:20:14
0:20:14
 0:07:50
0:07:50
 0:04:08
0:04:08
 0:03:39
0:03:39
 0:02:36
0:02:36
 0:10:44
0:10:44
 0:00:25
0:00:25
 0:00:16
0:00:16
 0:08:50
0:08:50
 0:02:52
0:02:52