filmov
tv
Respiratory Therapy - Airvo vs Salter HFNC

Показать описание
Please subscribe, like and comment. Would love to hear what you think about the video. Also look for me on social media....
IG @respiratorycoach
Twitter @coachrrt
BEST WISHES!!!
IG @respiratorycoach
Twitter @coachrrt
BEST WISHES!!!
Respiratory Therapy - Airvo vs Salter HFNC
Respiratory Therapy - Airvo Discussion
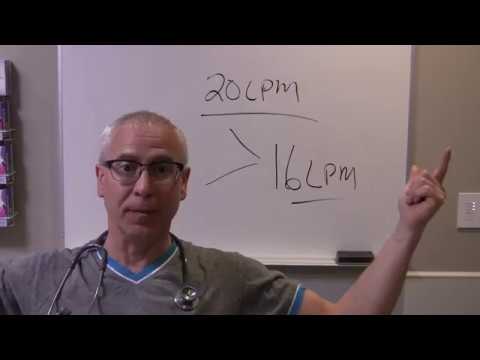
Low Flow versus High Flow Oxygen Therapy: The quick and the dirty
Oxygen Delivery Devices
Low Flow vs High Flow O2
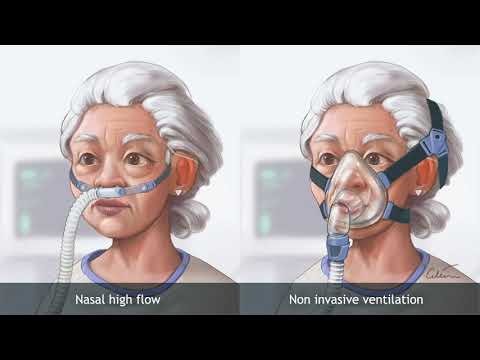
Nasal high‐flow therapy versus NIV in COPD patients with chronic respiratory failure
F&P Airvo 2 - Introduction
RT Clinic: Airvo 2 - Heated High Flow Oxygen Therapy
High Flow Nasal Cannula (Airvo, Vapotherm, Optiflow etc)
In2Flow Cannulas | How to use | High flow oxygen therapy
Airvo 2 High Flow Nasal Cannula Demonstration
High Flow Oxygen Therapy: Part 2 - Clinical application
High Flow Oxygen Therapy - Kiley Hodge, RRT, ACCS
Airvo High Flow Nasal Cannula
High Flow Oxygen Therapy: Part 1 - Introduction to HFT
RT Clinic : Heated High Flow Cannula
Respiratory Therapist - Oxygen Therapy: Nonrebreather Mask
Respiratory Therapy - What is Flow?
HFNC device introduction
Respiratory Therapy - BiPAP vs. CPAP - How to adjust for ABGs?
Airvo
High flow oxygen therapy with Hamilton Medical ventilators
Asthma and the Difference Between HVNI and HFNC
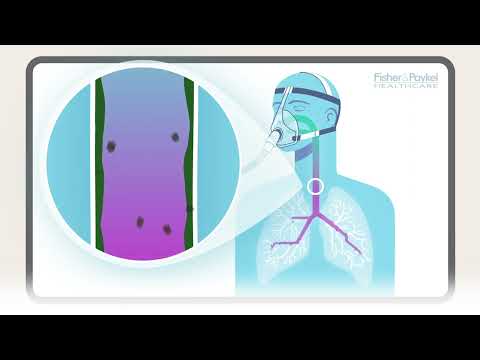
How does humidity support the lungs? | F&P Healthcare
Комментарии
 0:20:36
0:20:36
 0:20:30
0:20:30
 0:04:57
0:04:57
 0:19:24
0:19:24
 0:06:05
0:06:05
 0:03:04
0:03:04
 0:01:13
0:01:13
 0:16:59
0:16:59
 0:19:55
0:19:55
 0:02:19
0:02:19
 0:10:13
0:10:13
 0:04:15
0:04:15
 0:07:52
0:07:52
 0:22:41
0:22:41
 0:04:59
0:04:59
 0:11:31
0:11:31
 0:01:00
0:01:00
 0:19:25
0:19:25
 0:07:27
0:07:27
 0:20:58
0:20:58
 0:00:42
0:00:42
 0:01:59
0:01:59
 0:01:20
0:01:20
 0:02:21
0:02:21