filmov
tv
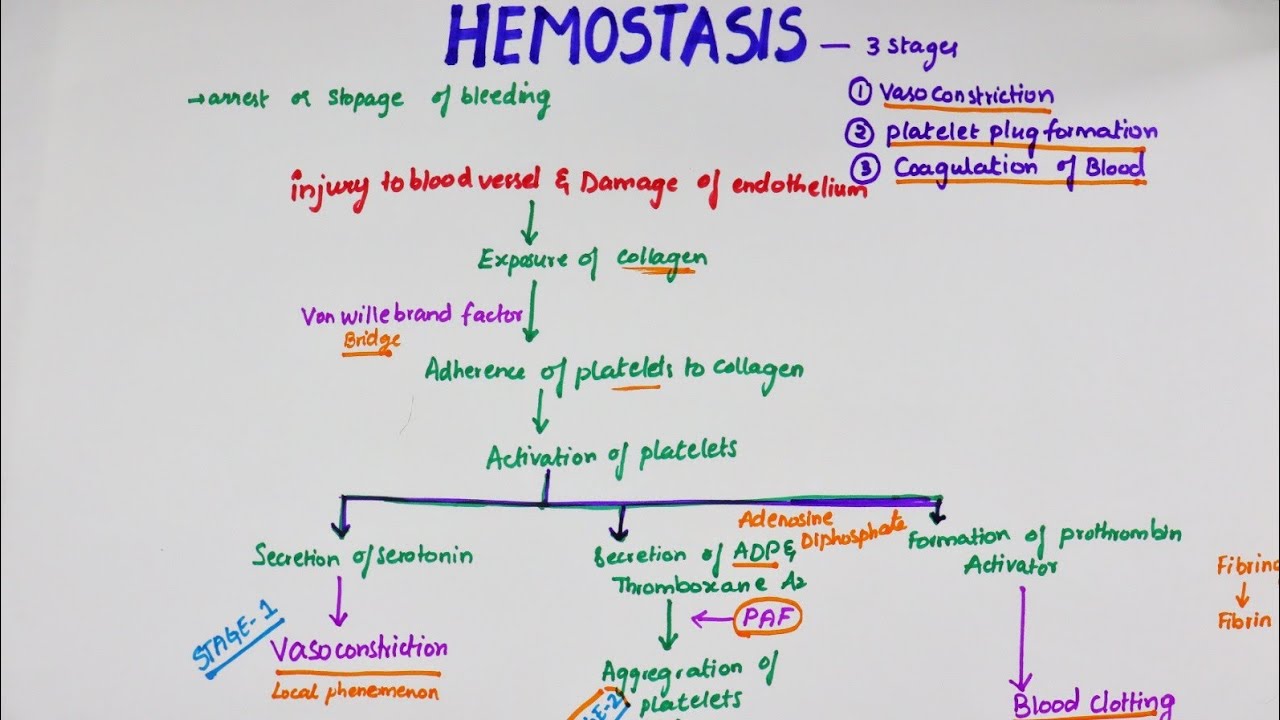
Hemostasis | Easy Flowchart | Physiology
Показать описание
Hemostasis or haemostasis is a process to prevent and stop bleeding, meaning to keep blood within a damaged blood vessel (the opposite of hemostasis is hemorrhage). It is the first stage of wound healing. This involves coagulation, blood changing from a liquid to a gel. Intact blood vessels are central to moderating blood's tendency to form clots. The endothelial cells of intact vessels prevent blood clotting with a heparin-like molecule and thrombomodulin and prevent platelet aggregation with nitric oxide and prostacyclin. When endothelial injury occurs, the endothelial cells stop secretion of coagulation and aggregation inhibitors and instead secrete von Willebrand factor, which initiate the maintenance of hemostasis after injury. Hemostasis has three major steps: 1) vasoconstriction, 2) temporary blockage of a break by a platelet plug, and 3) blood coagulation, or formation of a fibrin clot. These processes seal the hole until tissues are repaired.Hemostasis occurs when blood is present outside of the body or blood vessels. It is the innate response for the body to stop bleeding and loss of blood. During hemostasis three steps occur in a rapid sequence. Vascular spasm is the first response as the blood vessels constrict to allow less blood to be lost. In the second step, platelet plug formation, platelets stick together to form a temporary seal to cover the break in the vessel wall. The third and last step is called coagulation or blood clotting. Coagulation reinforces the platelet plug with fibrin threads that act as a "molecular glue".[3] Platelets are a large factor in the hemostatic process. They allow for the creation of the "platelet plug" that forms almost directly after a blood vessel has been ruptured. Within seconds of a blood vessel's epithelial wall being disrupted, platelets begin to adhere to the sub-endothelium surface. It takes approximately sixty seconds until the first fibrin strands begin to intersperse among the wound. After several minutes the platelet plug is completely formed by fibrin.[4] Hemostasis is maintained in the body via three mechanisms:
Vascular spasm (Vasoconstriction) - Vasoconstriction is produced by vascular smooth muscle cells, and is the blood vessel's first response to injury. The smooth muscle cells are controlled by vascular endothelium, which releases intravascular signals to control the contracting properties. When a blood vessel is damaged, there is an immediate reflex, initiated by local sympathetic pain receptors, which helps promote vasoconstriction. The damaged vessels will constrict (vasoconstrict) which reduces the amount of blood flow through the area and limits the amount of blood loss. Collagen is exposed at the site of injury, the collagen promotes platelets to adhere to the injury site. Platelets release cytoplasmic granules which contain serotonin, ADP and thromboxane A2, all of which increase the effect of vasoconstriction. The spasm response becomes more effective as the amount of damage is increased. Vascular spasm is much more effective in smaller blood vessels.[5][6]
Platelet plug formation- Platelets adhere to damaged endothelium to form a platelet plug (primary hemostasis) and then degranulate. This process is regulated through thromboregulation. Plug formation is activated by a glycoprotein called Von Willebrand factor (vWF), which is found in plasma. Platelets play one of major roles in the hemostatic process. When platelets come across the injured endothelium cells, they change shape, release granules and ultimately become ‘sticky’. Platelets express certain receptors, some of which are used for the adhesion of platelets to collagen. When platelets are activated, they express glycoprotein receptors that interact with other platelets, producing aggregation and adhesion. Platelets release cytoplasmic granules such as adenosine diphosphate (ADP), serotonin and thromboxane A2. Adenosine diphosphate (ADP) attracts more platelets to the affected area, serotonin is a vasoconstrictor and thromboxane A2 assists in platelet aggregation, vasoconstriction and degranulation. As more chemicals are released more platelets stick and release their chemicals; creating a platelet plug and continuing the process
Vascular spasm (Vasoconstriction) - Vasoconstriction is produced by vascular smooth muscle cells, and is the blood vessel's first response to injury. The smooth muscle cells are controlled by vascular endothelium, which releases intravascular signals to control the contracting properties. When a blood vessel is damaged, there is an immediate reflex, initiated by local sympathetic pain receptors, which helps promote vasoconstriction. The damaged vessels will constrict (vasoconstrict) which reduces the amount of blood flow through the area and limits the amount of blood loss. Collagen is exposed at the site of injury, the collagen promotes platelets to adhere to the injury site. Platelets release cytoplasmic granules which contain serotonin, ADP and thromboxane A2, all of which increase the effect of vasoconstriction. The spasm response becomes more effective as the amount of damage is increased. Vascular spasm is much more effective in smaller blood vessels.[5][6]
Platelet plug formation- Platelets adhere to damaged endothelium to form a platelet plug (primary hemostasis) and then degranulate. This process is regulated through thromboregulation. Plug formation is activated by a glycoprotein called Von Willebrand factor (vWF), which is found in plasma. Platelets play one of major roles in the hemostatic process. When platelets come across the injured endothelium cells, they change shape, release granules and ultimately become ‘sticky’. Platelets express certain receptors, some of which are used for the adhesion of platelets to collagen. When platelets are activated, they express glycoprotein receptors that interact with other platelets, producing aggregation and adhesion. Platelets release cytoplasmic granules such as adenosine diphosphate (ADP), serotonin and thromboxane A2. Adenosine diphosphate (ADP) attracts more platelets to the affected area, serotonin is a vasoconstrictor and thromboxane A2 assists in platelet aggregation, vasoconstriction and degranulation. As more chemicals are released more platelets stick and release their chemicals; creating a platelet plug and continuing the process
Комментарии