filmov
tv
Cardiac Resynchronization Therapy - Implantation Technique and CRT Implantation Pearls from Experts

Показать описание
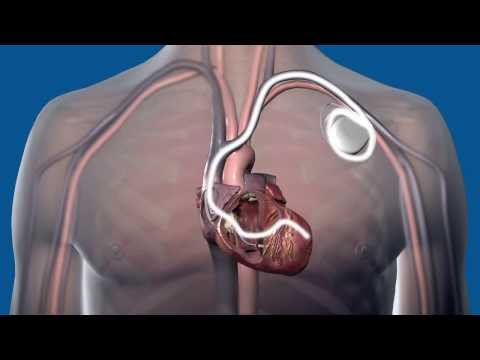
Continuation on cardiac resynchronization therapy. Moving on to technique of CRT implantation.
Basic cannulation of coronary sinus: Start ventricular to tricuspid valve and withdraw applying counter clockwise torque to stay septally to cannulate the coronary sinus ostium. LAO is lined upon the interventricular septum. The orthogonal view is RAO.
A prominent Thebesian valve with an associated pouch causes the lead to fall into it and cause difficulty in cannulating the coronary sinus. Injecting a whiff of dye will help delineate the position of the sheath in the pouch, which causes transient dye stasis.
Inability to advance in CS could be due to stenosis, valves, subselection, dissection and tortuosity. Vieussens valve is an embryonic remnant, seen at the origin of the posterolateral ventricular vein. If there is a prominent valve in the posterolateral vein, we can cannulate the middle cardiac vein and go into a lateral branch of this vein.
CS stenosis can be balloon dilated, but branch vein stenosis is better left alone. Search for other veins which could be used. This will also reduce the dye load in attempted dilatation. Dissections can occur due to dye injections and by sheath advancement.
In most of the dissections it is still possible to get a wire across and proceed. Otherwise if the dissection is distal, try using the lateral branch of the middle cardiac vein. Pushing a catheter which is sub selected without recognizing it is one of the reasons for dissection.
If it is atrial vein subselection, withdraw it. If it is ventricular vein subselection, your cannulation is over! So, try to recognize it with appropriate views.
In case of inability to get to lateral veins through a posterolateral vein, try lateral branches of middle cardiac vein or anterior interventricular vein. It is not important how you reach the lateral wall. The ideal site to aim for the left ventricular lead is the lateral wall, mid position.
Need for ICD lead in left ventricle: When there is a mechanical tricuspid valve which you don’t want to cross, an ICD lead may have to be placed in a coronary vein.
CRT implantation pearls from experts: Screw in lead for LV pacing can be used only if the sheath can be taken deep down into the vein as it is not introduced over a guide wire. If after screwing in, the lead has a high impedance and the threshold is high, it is likely to be on the pericardial side of the vein.
It may be unscrewed, and another position sought. Screw tip is only 1 mm and may not produce significant bleeding on unscrewing from the pericardial side. Screwing to the myocardial side typically shows ST elevation on the lead tip electrogram due to the injury current.
If threshold is not good, electronic configuration with pacing from proximal electrode or other combinations can be tried to improve efficacy. Issue with previous active fixation leads were that future removal or repositioning was not possible and they were also unipolar, preventing electronic configuration of pacing.
Unlike in conventional pacing where we want to minimize ventricular pacing, in CRT we want full biventricular pacing to occur. This may mean programming shorter AV delay to prevent intrinsic conduction. Inappropriately long AV delay can also cause a tendency for MR.
E-A fusion can cause diastolic MR, which in turn can worsen heart failure. Unduly short AV delay causes A wave truncation, which can also be associated with MR.
Intra-atrial conduction delay due to atrial fibrosis can increase AV delay. Atrial septal pacing is useful in reducing intra-atrial conduction delay.
Biatrial pacing is another option to synchronise the atria. Drug therapy to slow AV conduction and prevent fusion is also useful to improve biventricular pacing in CRT. Echo guided optimisation of AV delay is also possible (Ritter’s method).
During V-V delay optimisation, in some cases an LV offset causing pre-excitation of the LV may improve cardiac output. In interventricular dyssynchrony RV ejects at LV end diastole.
Intraventricular dyssynchrony is manifest as QRS onset to pulmonary ejection compared to aortic ejection of more than 40 ms, septal to posterior wall delay of more than 160 ms or septal to lateral wall delay of more than 60 ms in TVI.
3D synchronization is with colour coding of early and late contracting segments – early as green and late as red.
Maximum tracking rate has to be increased as heart failure status improves. This is for consistent pacing at higher rates needed during more activities permitted by better effort tolerance.
Transient worsening of renal function may be seen after CRT implantation due to the long procedure time. This may also cause worsening of heart failure.
The longer procedure time also enhances the chances for infection. Subclavian vein thrombosis is another potential problem due to the presence of three leads and a sluggish circulation due to heart failure. Look out for the next video in this series soon.
Basic cannulation of coronary sinus: Start ventricular to tricuspid valve and withdraw applying counter clockwise torque to stay septally to cannulate the coronary sinus ostium. LAO is lined upon the interventricular septum. The orthogonal view is RAO.
A prominent Thebesian valve with an associated pouch causes the lead to fall into it and cause difficulty in cannulating the coronary sinus. Injecting a whiff of dye will help delineate the position of the sheath in the pouch, which causes transient dye stasis.
Inability to advance in CS could be due to stenosis, valves, subselection, dissection and tortuosity. Vieussens valve is an embryonic remnant, seen at the origin of the posterolateral ventricular vein. If there is a prominent valve in the posterolateral vein, we can cannulate the middle cardiac vein and go into a lateral branch of this vein.
CS stenosis can be balloon dilated, but branch vein stenosis is better left alone. Search for other veins which could be used. This will also reduce the dye load in attempted dilatation. Dissections can occur due to dye injections and by sheath advancement.
In most of the dissections it is still possible to get a wire across and proceed. Otherwise if the dissection is distal, try using the lateral branch of the middle cardiac vein. Pushing a catheter which is sub selected without recognizing it is one of the reasons for dissection.
If it is atrial vein subselection, withdraw it. If it is ventricular vein subselection, your cannulation is over! So, try to recognize it with appropriate views.
In case of inability to get to lateral veins through a posterolateral vein, try lateral branches of middle cardiac vein or anterior interventricular vein. It is not important how you reach the lateral wall. The ideal site to aim for the left ventricular lead is the lateral wall, mid position.
Need for ICD lead in left ventricle: When there is a mechanical tricuspid valve which you don’t want to cross, an ICD lead may have to be placed in a coronary vein.
CRT implantation pearls from experts: Screw in lead for LV pacing can be used only if the sheath can be taken deep down into the vein as it is not introduced over a guide wire. If after screwing in, the lead has a high impedance and the threshold is high, it is likely to be on the pericardial side of the vein.
It may be unscrewed, and another position sought. Screw tip is only 1 mm and may not produce significant bleeding on unscrewing from the pericardial side. Screwing to the myocardial side typically shows ST elevation on the lead tip electrogram due to the injury current.
If threshold is not good, electronic configuration with pacing from proximal electrode or other combinations can be tried to improve efficacy. Issue with previous active fixation leads were that future removal or repositioning was not possible and they were also unipolar, preventing electronic configuration of pacing.
Unlike in conventional pacing where we want to minimize ventricular pacing, in CRT we want full biventricular pacing to occur. This may mean programming shorter AV delay to prevent intrinsic conduction. Inappropriately long AV delay can also cause a tendency for MR.
E-A fusion can cause diastolic MR, which in turn can worsen heart failure. Unduly short AV delay causes A wave truncation, which can also be associated with MR.
Intra-atrial conduction delay due to atrial fibrosis can increase AV delay. Atrial septal pacing is useful in reducing intra-atrial conduction delay.
Biatrial pacing is another option to synchronise the atria. Drug therapy to slow AV conduction and prevent fusion is also useful to improve biventricular pacing in CRT. Echo guided optimisation of AV delay is also possible (Ritter’s method).
During V-V delay optimisation, in some cases an LV offset causing pre-excitation of the LV may improve cardiac output. In interventricular dyssynchrony RV ejects at LV end diastole.
Intraventricular dyssynchrony is manifest as QRS onset to pulmonary ejection compared to aortic ejection of more than 40 ms, septal to posterior wall delay of more than 160 ms or septal to lateral wall delay of more than 60 ms in TVI.
3D synchronization is with colour coding of early and late contracting segments – early as green and late as red.
Maximum tracking rate has to be increased as heart failure status improves. This is for consistent pacing at higher rates needed during more activities permitted by better effort tolerance.
Transient worsening of renal function may be seen after CRT implantation due to the long procedure time. This may also cause worsening of heart failure.
The longer procedure time also enhances the chances for infection. Subclavian vein thrombosis is another potential problem due to the presence of three leads and a sluggish circulation due to heart failure. Look out for the next video in this series soon.
 0:06:31
0:06:31
 0:05:35
0:05:35
 0:00:48
0:00:48
 0:02:03
0:02:03
 0:01:40
0:01:40
 0:02:51
0:02:51
 0:05:23
0:05:23
 0:21:31
0:21:31
 0:44:08
0:44:08
 0:00:48
0:00:48
 0:02:09
0:02:09
 0:00:51
0:00:51
 0:01:08
0:01:08
 0:01:30
0:01:30
 0:16:36
0:16:36
 0:00:03
0:00:03
 0:37:09
0:37:09
 0:03:29
0:03:29
 0:06:31
0:06:31
 0:02:03
0:02:03
 0:02:56
0:02:56
 0:01:44
0:01:44
 0:03:11
0:03:11
 0:10:38
0:10:38